Infertility
From imaging to clinical diagnosis
Exploring Female Fertility: central place of the ultrasound in first intention (Fertiliscan©)
Exploration, in search of the cause of infertility, is legally obligatory before any treatment is taken (Guide to Good Practice in Reproductive Medical Assistance (AMP) - Order of 30 June 2017(1) amending the Order of 11 April 2008(2)). It is essential to make the correct indications to the different techniques of AMP.
In fact, tubal exploration must be carried out immediately in the infertile couple balance, as must the spermogram. The tubal state is a limiting factor given its frequency and its impact on subsequent management. Thonneau et al. reports in a large French cohort that 26% of infertile women have tubal abnormalities(3).
Coelioscopy
The gold standard for tubal exploration is coelioscopy, with blue proof. It allows the diagnosis and treatment of endometriosis and peritubary adhesions.
However, this is an invasive and expensive technique, requiring general anesthesia, and Chapron et al. reported 0.5% surgical complications(4). The completion of a minimum surgery such that fertilization remains a surgical technique and is only available in certain establishments. Surgery is not suitable for routine examination in infertile women. She must remain an act of second intent when a woman has been detected at risk of abnormality.
Hysterosalpingography
The most commonly prescribed test is hysterosalpingography (HSG). In addition to assessing tubal permeability, HSG also provides an image of the uterine cavity. Given its relatively low cost, the HSG meets the criteria for a first-line review. However, it presents several risks: exposure to ionizing radiation (exposure of 2.05 Gy cm2, compared to 0.09 Gy cm2 for a thorax radiography), iodine allergy and infectious complication (peritonite). It also has the major disadvantage of being ill-tolerated because of pelvic pain when performing the examination. Finally, while its specificity is good for detecting a tubal abnormality or a bilateral tubary pathology of 87% and 95% respectively, its sensitivity is low, 53% and 46% respectively, compared to coelioscopy(5).
Envaginal ultrasound
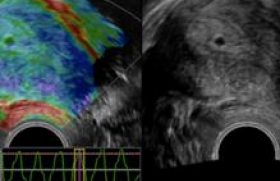
Thanks to technical improvement, endovaginal ultrasound is now more accurate than HSG to establish tubal permeability and has the added advantage of exploring the whole pelvis at the same time. Ultrasound, compared to HSG, also allows for better analysis of cavitary abnormalities.
Echography versus coelioscopy
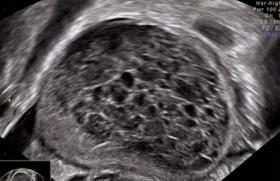
HyCoSy (hysterosalpingo-contrast-sonography) or HyFoSy (hysterosalpingo-foam-sonography) are very easily performed in the firm, without the need for radiology service or iodized contrast product. The ultrasound used for this procedure shall be equipped with a vaginal probe, preferably 3D, in order to obtain a perfect frontal cut for uterine exploration, and shall be equipped with a precise 2D imaging for the "tubal permeability" step. The training is readily available to any practitioner who usually performs endovaginal pelvic ultrasound and the examination is very well tolerated by the patients. Van Schoubroeck and al. showed that 48% of women felt that the test was not painful and 33% that the discomfort was identical to that of the basic vaginal ultrasound(6). As for comparison with HSG, a randomized controlled study by Dreyer et al.(7) shows that HyFoSy is both less painful, with an average analog visual scale (EVA) pain rating of 1.7 versus 3.7, and also has the advantage of being faster, with a duration of 5 minutes versus 12.5 minutes for HSG.
Comparative techniques
The HyCoSy is made with serum and air (contrast), while the HyFoSy is made with a sparkling gel (foam), which provides better air stability in the gel for contrast during the examination. A very well-conducted observational study by Ludwin et al.(8) compared HyCoSy and HyFoSy with methylene blue coelioscopy test in 132 women (259 trumps), each with 3 examinations. Patients were not selected and the prevalence of tubal obstruction in the population was 6.9% of the tubes. This study found an excellent negative predictive value of 99% for the 2 ultrasound tests, i.e. the evidence of a tubal passage with HyCoSy or HyFoSy corresponds to a permeable tube confirmed by the blue test.
HyCoSy or HyFoSy?
However, the positive predictive value of HyCoSy was significantly lower than that of HyFoSy (30% versus 71%), resulting in more inconclusive or no tubal examination with HyCoSy, while the blue is positive. The use of gel (Exem® gel) therefore improves the sensitivity of the examination. The HyFoSy should therefore be preferred in the first place, or systematically realized in the event of a tubal passage not being revealed with the HyCoSy. Given the safety of the gel, HyFoSy should be done at the outset, although some authors(8) proposed to do so as a second-line after HyCoSy, with the patient’s pain or discomfort proportional to the amount of fluid injected(9).
A Time for Everything
Like HSG, HyFoSy must be performed at a specific time in the cycle, to avoid the risk of exposure to a pregnancy and, on the other hand, because of the higher risk of false positive (clogged trunk) in the event of an overly thick endometrium, making it difficult for the gel to pass through the ostium. It is therefore recommended that this examination be carried out after the end of the rules and before the excessive proliferation of the endometrium, i.e. between J5 and J9.
If a lack of passage is found with a thick endometrium, given the good tolerance of the examination, it is possible to reprogram it at the very beginning of the follicular phase of the next cycle, thus avoiding a more invasive complementary exploration. In the case of tubal passage, given the almost 100% specificity of HyFoSy, the trumps may be considered functional and it is not necessary to carry out a further examination.
As a last resort for fertility exploration
In the event of an anomaly, the decision to carry out a complementary coelioscopy must take into account the age of the woman, the history and duration of infertility, as well as the spermogram of the spouse, which must also be carried out at the forefront of the exploration of the infertile couple. In some cases, especially age-related, given the reduced chance of spontaneous fertility, blue-proof coelioscopy has less interest in its benefit-cost ratio. Under these conditions, it is preferable to direct the couple from the outset towards the realization of in vitro fertilization (IVF). Several authors, such as Lim et al., suggest that HSG no longer has a place in modern exploration of infertile women(10).
Post-ultrasound steps
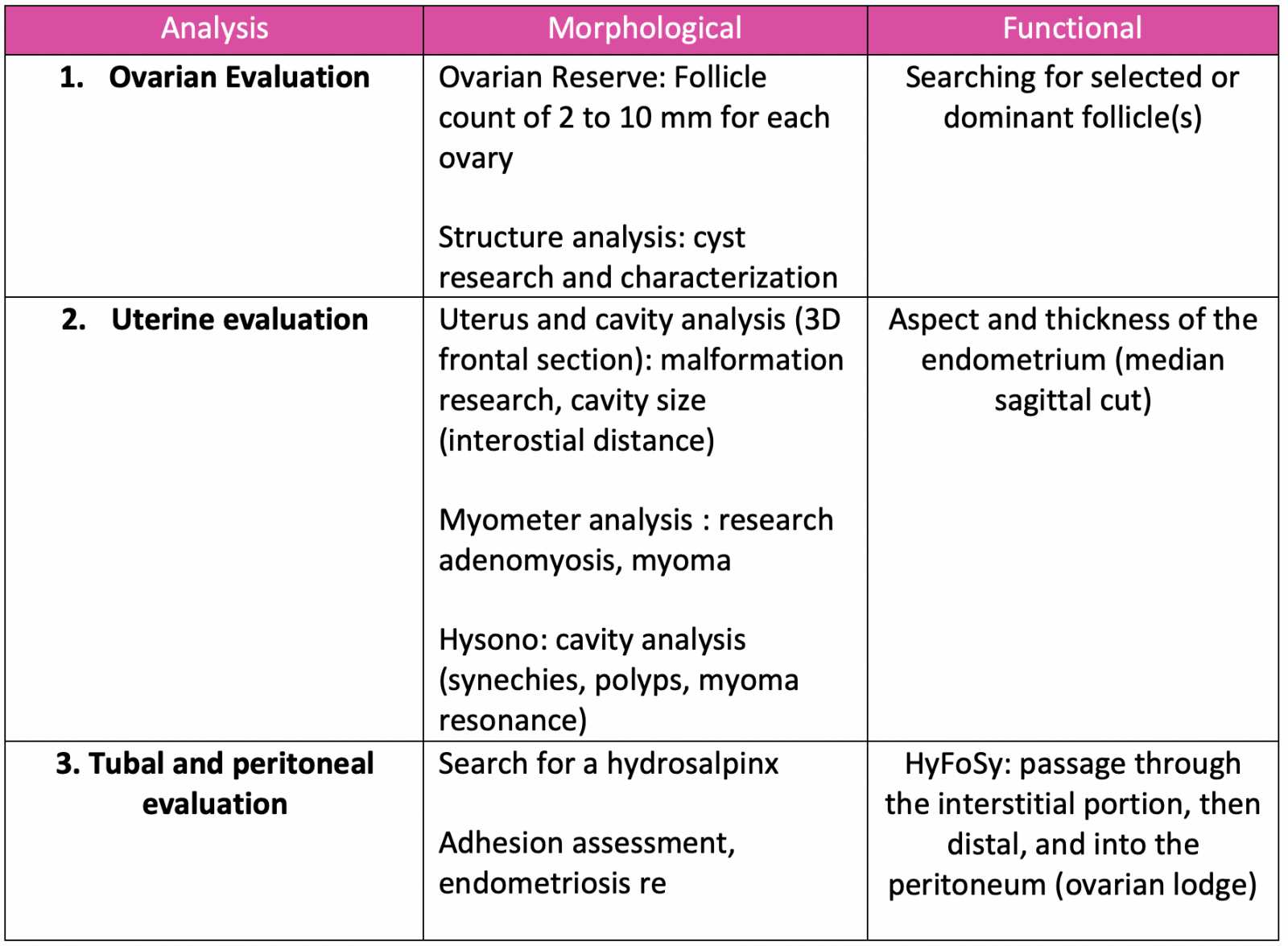
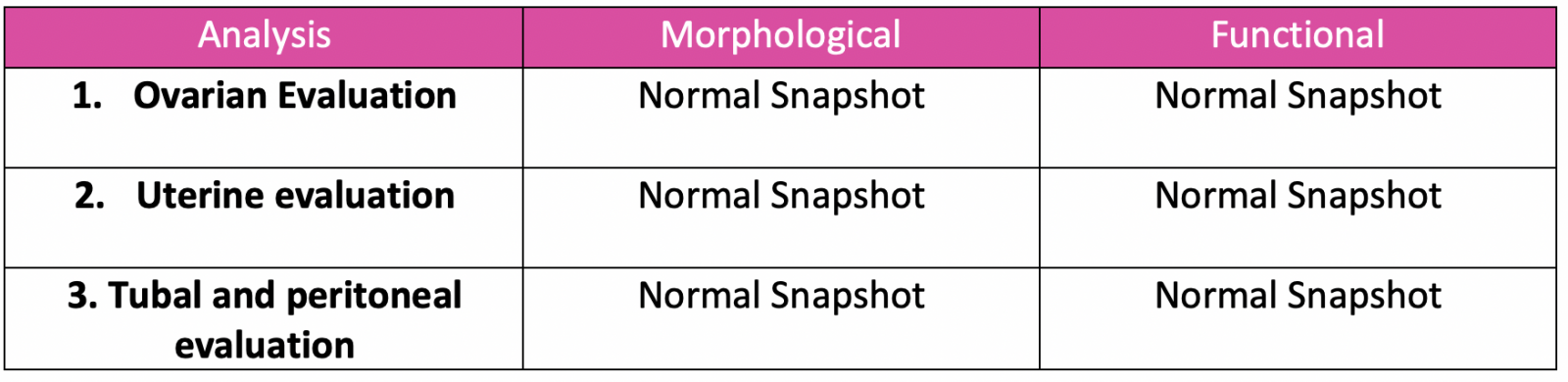
The advantage of the first-line ultrasound is not only its reliable and rapid exploration of tubal permeability, but also the very precise evaluation of the uterus and uterine cavity and the annexes. Thus, with a well-conducted examination, the clinician has a precise analysis, both morphological and functional, of ovaries, uterus and trumps, allowing him to direct possible further explorations, or from the outset a care in medical assistance for reproduction. The graph below summarizes the "modern" exploration of the infertile couple in 2017.
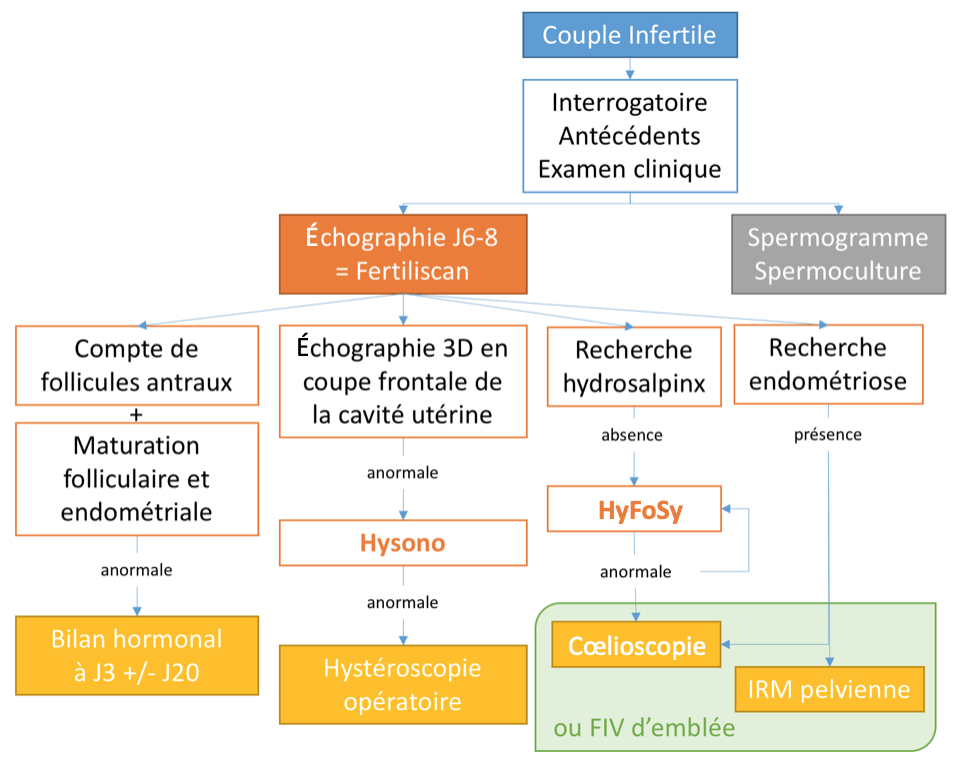
Infertile Couple → Background questions and clinical review
Echograph J6-8 = Fertiliscan | Spermogram Spermoculture
Antral follicle count + Follicular and Endometrial Maturation : not normal → Hormonal balance at J3 +/- J20
3D ultrasound in the frontal section of the uterine cavity : not normal → Hysono : not normal → Operative Hysteroscopy
Hydrosalpinx Research : abscence → HyFoSy : not normal → Coelioscopie (or IVF from the beginning)
Endometriosis Research : Presence → Coelioscopie or MRI pelvic (or IVF from the beginning)
Fertiliscan©
The first-line ultrasound in the infertility check, or Fertiliscan ©, is performed in 3 stages, taking a total of 30 minutes and can be performed in the firm. It saves the couple several weeks, i.e. 1 h versus 13 weeks for a "classic" exploration, and also has an obvious financial advantage, with a cost ranging from single to triple(11).
The examination begins with an endovaginal pelvic ultrasound that will evaluate the ovaries and the pelvis as a whole, and ensure that there is no contraindication to an intrauterine injection, in particular the existence of a hydrosalpinx. The endovaginal probe is then removed to place the speculum and place a catheter (e.g. Elliocath® transfer catheter®, with or without a contention system) at the inner hole of the cervix, mounted with a syringe containing physiological serum. Speculum is then replaced by the endovaginal probe and hysterosonography (Hysono) is performed to evaluate the uterine cavity. In the process, the serum remaining in the cavity is sucked and the syringe is replaced by a syringe containing Exem® gel. The catheter is pushed to the bottom of the uterine cavity and the HyFoSy is realized. A standard report is then provided to the patient. It must contain all the elements mentioned in the table below, with the corresponding echographic shots.
In 2017, endovaginal pelvic ultrasound is a must-see when exploring infertility in women. It should be performed by a practitioner trained in the specific exploration of fertility. Its place is on the front line in the diagnostic strategy and then makes it possible to direct towards additional explorations if necessary, or immediately towards a technique of medically assisted procreation.
Hervé Fernandez : membre du board Bayer
Hervé FERNANDEZ1,2,3, Solène VIGOUREUX1,4, Anne-Gaëlle POURCELOT1, Perrine CAPMAS1,2,3, Le Kremlin-Bicêtre
1. AP-HP, CHU Bicêtre, Service Gynécologie Obstétrique, Le Kremlin-Bicêtre, France
2. Faculté de Médecine Paris-Sud Saclay, Le Kremlin-Bicêtre, France
3. CESP-INSERM U1018 « Reproduction et Développement de l’enfant », Le Kremlin-Bicêtre, France
4. CESP-INSERM U1018 « Genre, Sexualité et Santé », Le Kremlin-Bicêtre, France
References
Click on the references and access the Abstracts on

1. Arrêté du 30 juin 2017 modifiant l’arrêté du 11 avril 2008 modifié relatif aux règles de bonnes pratiques cliniques et biologiques d’assistance médicale à la procréation. Search the abstract2. Arrêté du 11 avril 2008 relatif aux règles de bonnes pratiques cliniques et biologiques d’assistance médicale à la procréation. Search the abstract3. Thonneau P et al. Incidence and main causes of infertility in a resident population (1 850 000) of three French regions (1988–1989)*. Hum Reprod 1991 ; 6 : 811-6. Search the abstract4. Chapron C et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod Oxf Engl 1998 ; 13 : 867-72. Search the abstract5. Broeze KA et al. Are patient characteristics associated with the accuracy of hysterosalpingography in diagnosing tubal pathology? An individual patient data meta-analysis. Hum Reprod Update 2011 ; 17 : 293-300. Search the abstract6. Van Schoubroeck D et al. Pain during Fallopian-tube patency testing by hysterosalpingo-foam sonography. Ultrasound Obstet Gynecol 2015 ; 45 : 346-50. Search the abstract7. Dreyer K et al. Hysterosalpingo-foam sonography, a less painful procedure for tubal patency testing during fertility workup compared with (serial) hysterosalpingography: a randomized controlled trial. Fertil Steril 2014 ; 102 : 821-5. Search the abstract8. Ludwin I et al. Accuracy of hysterosalpingo-foam sonography in comparison to hysterosalpingo-contrast sonography with air/saline and to laparoscopy with dye. Hum Reprod 2017 ; 32 : 758-69. Search the abstract9. Socolov D et al. Comparison of the pain experienced by infertile women undergoing hysterosalpingo contrast sonography or radiographic hysterosalpingography. Int J Gynaecol Obstet 2010 ; 111 : 256-9. Search the abstract10. Lim CP et al. Should a hysterosalpingogram be a first-line investigation to diagnose female tubal subfertility in the modern subfertility workup? Hum Reprod 2011 ; 26 : 967-71. Search the abstract11. Hrehorcak M, Nargund G. “One-Stop” fertility assessment using advanced ultrasound technology. Facts Views Vis ObGyn 2011 ; 3 : 8-12. Search the abstract
Articles on the same theme
- 1 of 5
- >