Non-oncologic gynecology
From imaging to clinical diagnosis
Confrontation between preoperative ultrasound and surgery
The purpose of any pre-operative imaging is the finest possible approach to diagnosis for a high-quality initial surgical strategy. Ultrasound, with its many tools, is capable of addressing the whole of utero-ovarian disease. This is the essential, and often the only, prerequisite for a well-considered and prepared surgery. Very rarely insufficient or incomplete, it will allow the patient to be directed to another type of imaging, mainly MRI.
Prevented from any peroperative contingencies (diagnostic correction, pathway conversion or surgical adjustment itself), the patient has a clear moral and medico-legal contract.
The volumic approach and, more recently, the elastography have opened the way to echo-endoscopic imaging and "digital palpation." We thus access within the cystic lesion or endometrial cavity without being invasive, and to the indirect palpation of the lesions, in the hippocratic sense of the term.
This finesse of examination is such that we gradually move from a positive, descriptive, sometimes gross diagnosis, to a real presumption of the nature of the histological process.
The initial study of the lesion But this should be done without any preconceptions about the histological result, regardless of our experience, because there are many traps. Our approach will consist of an extremely accurate 2D descriptive analysis (size, wall, vegetation, locularity, intraperitoneal effusion, vascularization, etc.) before taking the next step, with two particularly powerful tools: the volumic approach and the elastography.
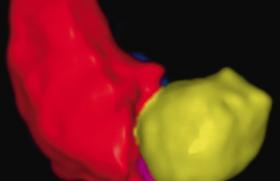
The volumic approach
This approach brings another, complementary look, with a simplified anatomical finding since we simultaneously have the volume, its three reference planes, and all the time needed to work afterwards without hindering the patient. The possibility of saving volumes will allow a secondary study, identical to that of real time, and offers the possibility of using a reference.
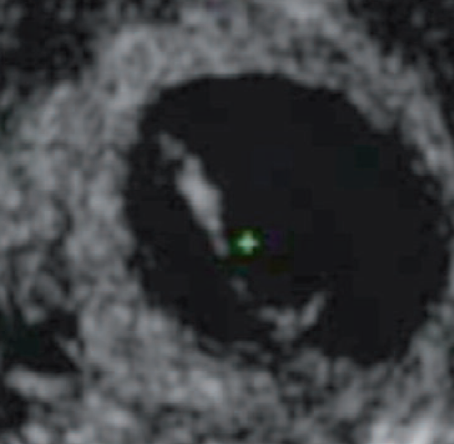
The exploitation of the volume will be (Figure 1):
- or by navigation in the volume, which sometimes reveals a wall not visualized in 2D (possibility of KIP for the surgeon), an ill-defined thickness and irregularity, a vegetation that can change everything, partitions including thickness, layout and flexibility are expressed differently. The remaining functional ovarian zone is better identified and quantified. The proportion between the internal structures of the cyst is clearly established;
- either by the analysis in the surfacial mode and it is a real revolution in the approach of cystic lesions.
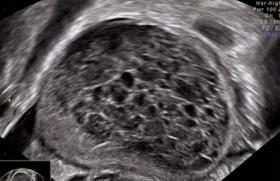
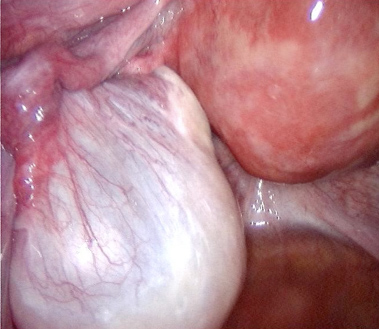
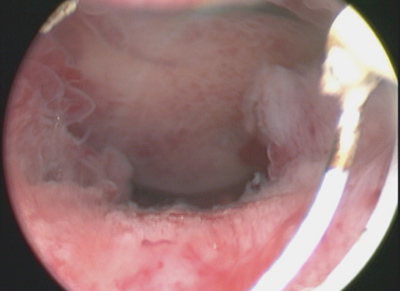
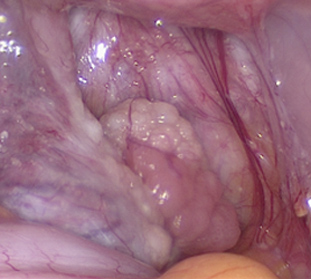
We thus access the "virtual cystoscopy". This cystoscopy is extremely precise and the aspects described are superposable to those found during coelioscopy. Installed within the cystic image itself, we can, at will, take the time of a thorough analysis (Figures 2 and 5 to 8).
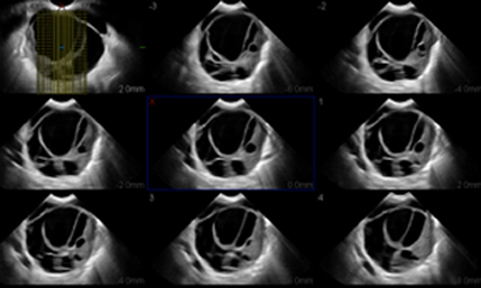
Figure 1: Multi-section navigation.
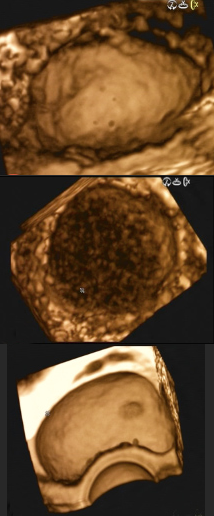
Figure 2: Virtual Kystoscopy.

Figures 5 and 6: Surface vegetation and macroscopic vegetation. The virtual endoscopic aspect of vegetation is superposable to the macroscopic aspect.
Figures 7 and 8: Virtual Kystoscopy visualizing perfectly the inner surface of the wall with folds and vegetation. Peroperatory cystoscopy is perfectly correlated with the ultrasound image.
• Cystoscopy easily corrects the diagnosis for an aspect of pseudo-vegetation or partition, mimicked by a simple clot or fibrinar organization (Figures 3 and 4).
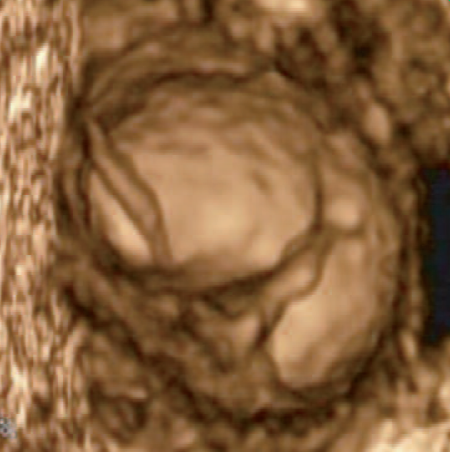
Figures 3 and 4: Deceptive appearance of bulkhead, easily corrected by 3D surface (fibrinar organization).
It should be recalled that approximately 10-15% of our coelioscopies are made for functional images whose initial ultrasound appearance may mislead the diagnosis (Figures 5 and 6).
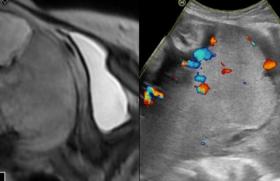
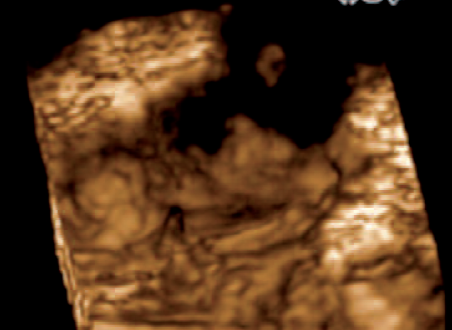
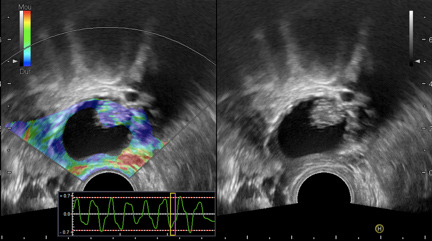
• The vascularization study also benefits from this 3D approach (Figures 9-12).
• Similarly, endometrial pathology benefits from this volumic approach and a A real virtual hysteroscopy, magnified by the fluid contrast, will precede the surgical hysteroscopy.
The 3D echo allows the front cut of the uterus with all its advantages. It is very easily obtained from a sagittal cross-section with an adequate scanning angle (Figures 13 and 14).

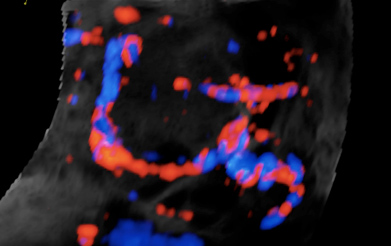
Figures 9 and 10: Vascularization rather peripheral of the functional images.
Figures 11 and 12: Vascularization in comb from the hilt for organic lesions.
Figures 13 and 14: Polyp in sagittal and frontal cuts.
All endocavity lesions or those that affect the cavity are easily visible (accurate mapping of polyps, endocavity and submucosa myomes) with a large amount of information for the surgeon. The myometer and its thickness are also well visible, as well as the appearance of the uterine bottom and the pore portion of the trumps.
Essential in the uterine malformations, it will easily make the differential diagnosis between a uterine partition (length of the partition, safety distance with the serum for resection, vital information for the surgeon, etc.) and a bicorn uterus.
The frontal cut also prepares the gesture before laying tubal implants or allows the verification of the position of an IUD.
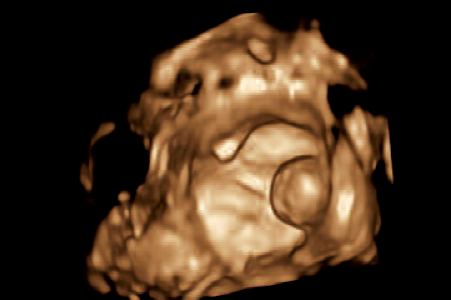
The following example illustrates the correlation between virtual hysteroscopy and surgical hysteroscopy (Figures 15 and 16).

Figures 15 and 16: Virtual and operative hyposteroscopy.
The use of the volume in the surface and multisection allows to assess the volume of a polyp or myoma, the location of its pedicle, vascularization, the endometrium junction, etc., all of the essential information for the surgeon (figures 17 to 19).
The input of these virtual endoscopies places us in the conditions of the real operatic speech. Our pre-operative diagnosis increases in sensitivity and specificity, so the initial operative strategy is better defined.

Figures 17, 18 and 19: Front cut polyp + surface rendering and its peroperative aspect. Perfect correlation between 3D/surface representation and macroscopy.
Elastography
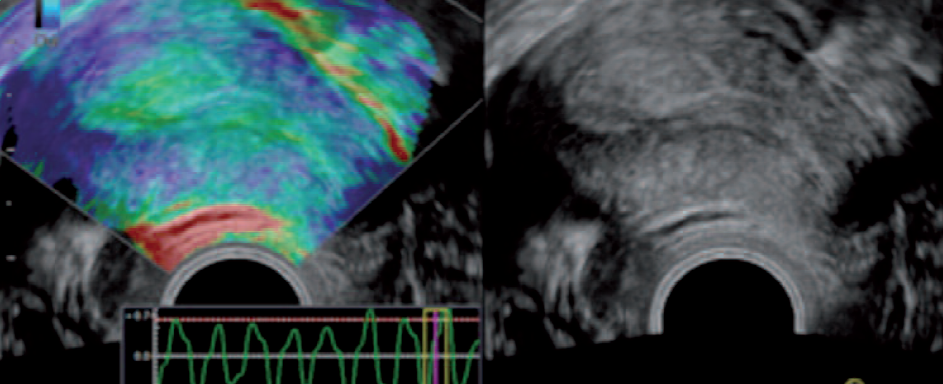
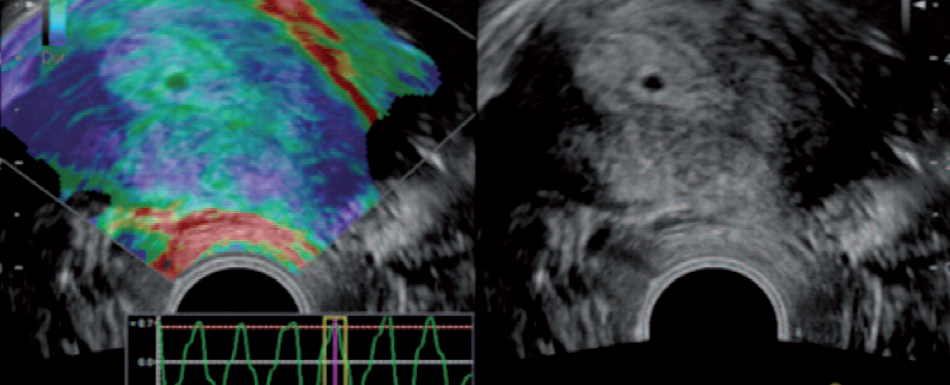
His early stages in gynecology seem promising. It allows an "ultrasonic touch" by assessing the elasticity of the tissues. After successive compression, a color code, ranging from blue (hard) to red (soft), superimposed on the 2D image, determines a precise mapping of the elasticity differences. It objectifies tissue changes and makes it possible to suspect any early tissue disorganization of an invaded structure.
The correct interpretation of images therefore requires, as with 2D, the perfect knowledge of physiological cyclic changes.
For ovarian cysts, all information useful for the surgeon is available in pre-operative ultrasound (wall or not, internal structures, vascularization, intraperitoneal effusion al, etc.) but one, although the most important to know: the notion of capsular rupture (Figure 20).
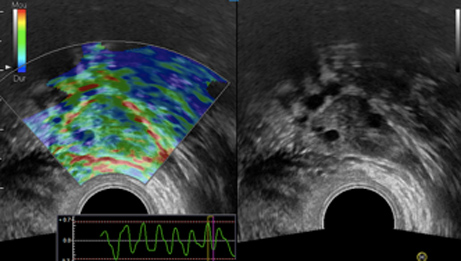
Figure 20: The capsule of a healthy and non-adherent ovarian is clearly visible, underlined by a red border.
In the following case, the capsular rupture is suspected before the loss of the red margin. Macroscopic observation confirms capsular rupture with an astonishing correlation of precision. The endokystic vegetation is appreciated in its volume, its implantation, its location on the inner wall, but also its hardness (the larger the vegetation, the more vascularized the softer it is red with elastography, the more suspect it is) (Figures 21 and 22). Each type of organic cyst has a particular appearance in elastography, which improves the prediction of histological diagnosis.
Endometrioma, for example, has a pathognomonic aspect as in 2D, but elastography provides important additional information: confirmation of adhesion with neighboring organs and their surface. The degree of infiltration, particularly interesting to know in the nodules of the double-vaginal bulkhead, is not always easy to highlight in 2D; color mapping specifies the depth of infiltration and its limits with the digestive (figure 23). The technique makes it possible to distinguish an aged endometrioma (more difficult cleavage, adaptation of the technique (laser spray, KIP), always with the greatest respect for the follicular capital - all fundamental information for the surgeon - (Figure 24).
Figures 21 and 22: Endocratic vegetation. Capsular break, macroscopic.
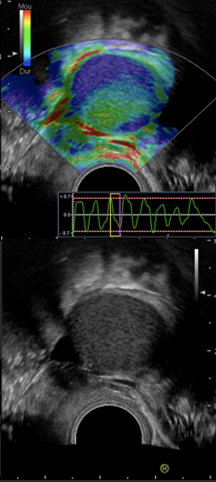
Figure 23: Young endometrium in elastography.
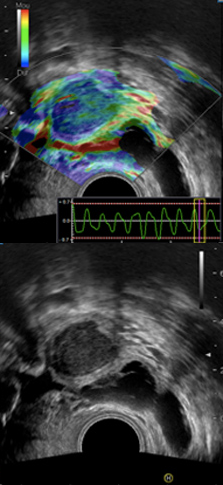
Figure 24. Changes in aging endometrioma.
The elastographic analysis of the endometrium also requires knowledge of cyclic physiological changes to be well interpreted. They are superposable to those observed in 2D. These different aspects reflect histological changes in estrogen progestin impregnation (Figures 25 to 27).
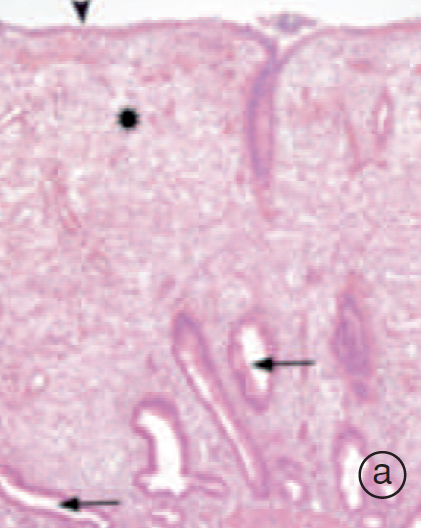
Figure 25a: proliferative phase endometers.
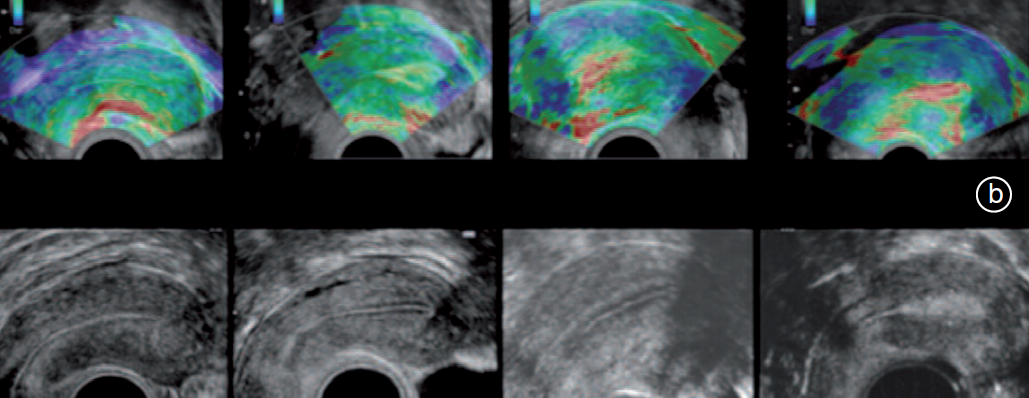
Figure 25b: Normal endometrium elastography during a cycle based on glandular changes.
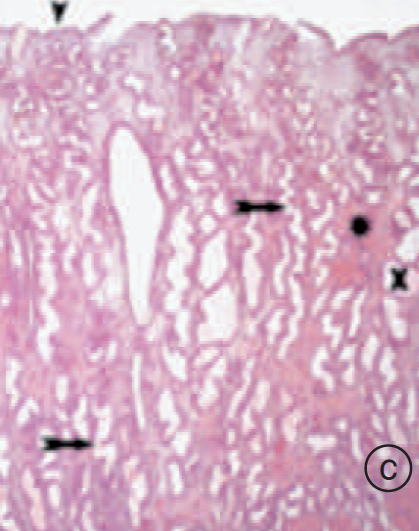
Figure 25c: Endometer secretory phase.
Figures 26 and 27: Glaandulo-cystic polyp in elastography.
The interests of elastography in this field are numerous: fluid contrast is no longer required for initial diagnosis of endocavity lesions, which is particularly interesting when there is little difference in contrast between endocavity and normal endometrium (polyp in a secretory endometrium) or if no nursery vessel is visualized, or when the cervix is not catherisable in some menopausal patients. Changes in color mapping indicate the lesion from the outset and even appreciate the nature of the histological process.
The elastography also allows us to assess the quality of the myometer. While 2D and 3D echo is largely sufficient for the diagnosis of adenomyosis or myomas (with the exception of large or multiple myomas), it is insufficient to detect myometer alteration and its impact on fertility. The aging or alteration of its various tissue components changes the uterine elasticity and color mapping.
Conclusion
• The volumic approach associated with elastography offers new perspectives. Of course, forward-looking, multi-center evaluations will be essential to verify these initial results.
• Our pre-operative diagnosis now begins, with all due care, with "histological presumptions".
• The initial operational strategy is well prepared, well thought out. The surgical procedure will be respectful of follicular capital when treating benign organic ovarian masses, or, on the contrary, will indicate the realization, in one moment, of a radical gesture of which the patient has been warned.
• The best way forward is by confronting, for each case, the ultrasonists and surgeons with their pre- and peroperative data first, and then with the anatomopathological results.
• Dialog is essential if we are to respect the unique physiology of each of our patients, to preserve their fertility and their anatomical integrity.
• Surgery feeds on the richness of the information provided by ultrasound imaging, and in turn, peroperative findings improve the understanding of images.
• Thus, it is time and logical to integrate vaginal ultrasound in the continuity of our clinical examination as it turns this tool into a real reader of anatomy or individual pathology.
Articles on the same theme
- 1 of 5
- >