Gynecologic emergencies
Can we do without Doppler color in gynecological ultrasound?
Can we imagine an ultrasound examination in gynecology without using color Doppler ? For many of us the question is rhetorical, but for others in Europe the answer seems to be much more mixed. Recently, at congresses both in the Netherlands and in the UK, some speakers seemed to doubt the contribution of color Doppler. And it is with a unifying purpose that the IOTA Group decided not to include color criteria in their latest system of prediction of ovarian masses (Timmerman et al. 2000; Van Calster et al. 2015).
But can we still doubt the contribution of color Doppler to gynecology? Some examples.
Deep endometriosis or rectum tumor ?
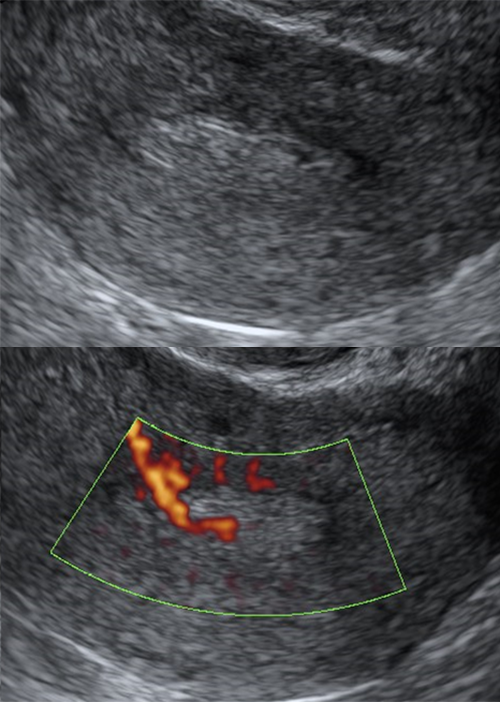
In Figure 1, a hypoechogenic nodule is seen in the front wall of the rectum. The nodule is slightly irregular and appears to be in continuity with the rectum muscle wall. The ultrasound image may suggest a rectum endometriosis nodule (Guerriero, Condous et al. 2016). However, at the color Doppler, the lesion is strongly vascularized. This makes the diagnosis of endometriosis difficult, as the endometriosis nodule is typically little or no vascularized. The final diagnosis of the lesion was a metastasis of endometrial cancer that occurred ten years after hysterectomy (Vangoitsenhoven et al. 2017).
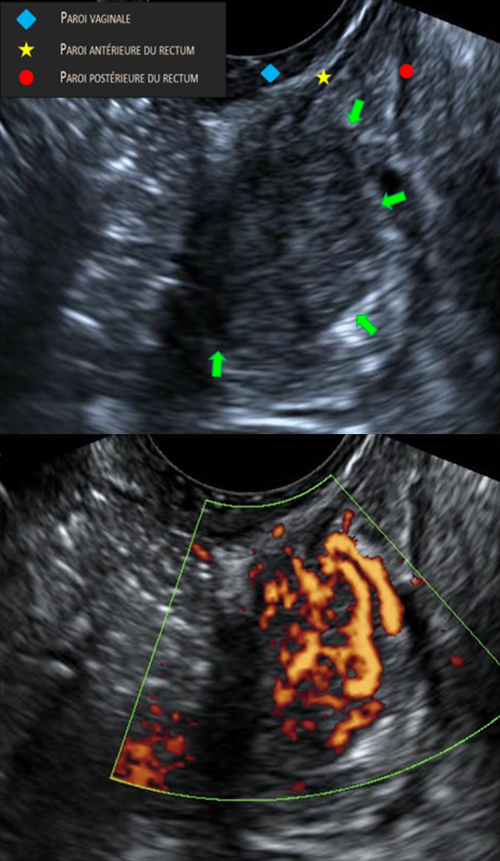
♦ Vaginal Wall Earlier
☆ Anterior rectum Wall
⇒ Posterior rectum Wall
Figure 1: Deep endometriosis or rectum tumor?
Cervical cancer ?
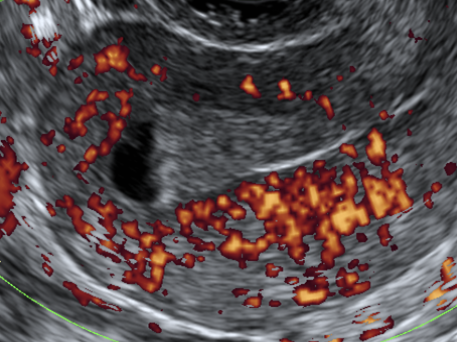
Cervical cancer has a similar ecogenicity to healthy cervical tissue. This makes the lesion difficult to determine on the black and white ultrasound examination (Figure 2). Spinocellular cancer is often low in ultrasound, while adenocarcinoma is frequently iso-ultrasonic compared to cervical tissue, making it even less detectable (Epstein et al. 2010). On the other hand, almost all cervical cancers are (strongly) vascularized, and therefore easily visible on the color Doppler examination.
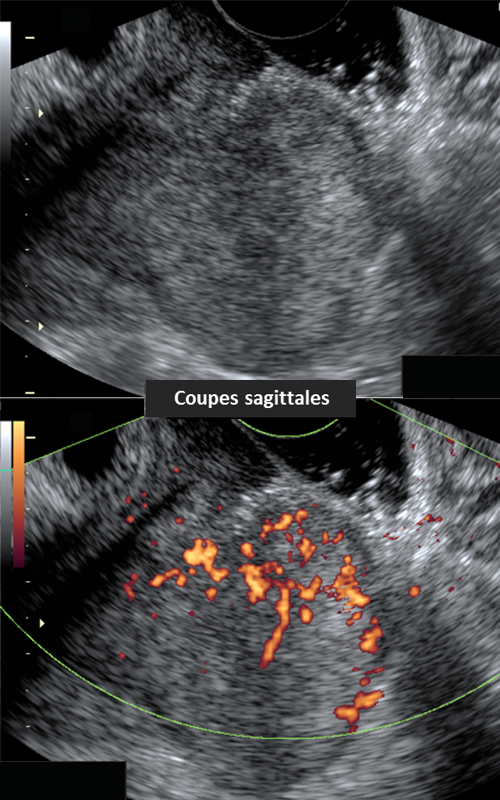
Sagittal Cuts
Figure 2a: Cervical cancer?
Transverse cuts
Figure 2b: Cervical cancer?
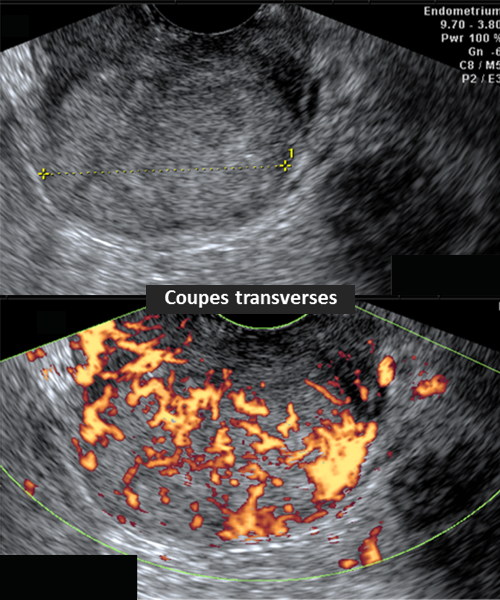
Trophoblastic residue or clot?
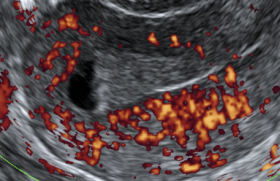
Detection of trophoblastic residue after curetting, miscarriage or delivery is often difficult to ultrasound in black and white. The lesion can easily be confused with a clot. If the Doppler examination is visualized, the clot is excluded, and the diagnosis of a trophoblastic residue is likely (Van den Bosch et al. 2008).
A blood sample to determine the HCG level may be confusing: a low or non-detectable HCG level only demonstrates the absence of functional trophoblastic tissue, but does not exclude the presence of trophoblastic tissue (Van den Bosch et al. 2002).
The presence of trophoblastic residue, however small, often stimulates the vascularization of the underlying myometer (Figure 3). Myometrial vessels can be prominent with high flow speeds. Once the residue has left (spontaneously or by surgical gesture), the vascularization of the underlying myometer will quickly normalize (Van den Bosch et al. 2015).
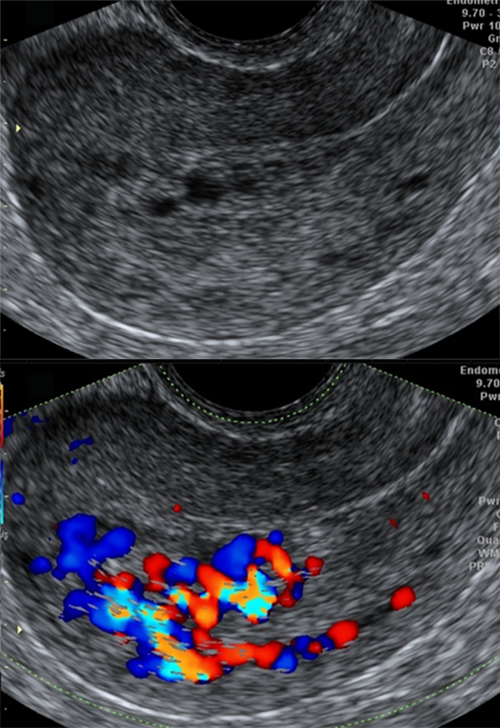
Figure 3: Trophoblastic residue or clot?
Liquid or solid?
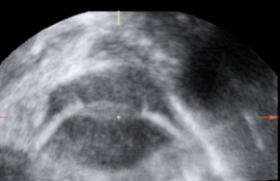
In black and white ultrasound, differential diagnosis of image lesion (Figure 4) tends to favor the endometrioma or hemorrhagic cyst of the ovary: rounded lesion with a hypoechogenic content of type sanded glass (Van Holsbeke et al. 2010).
But at the color Doppler, multiple vessels are visible, reversing the fluid nature of the lesion. Histological diagnosis is a fibrothecoma of the ovarian.
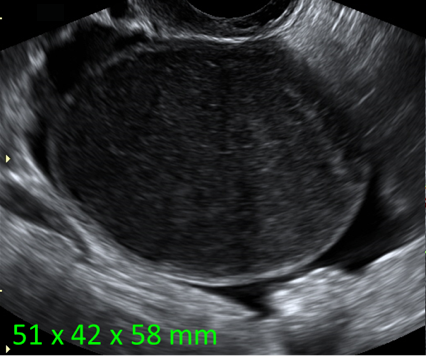
Figure 4a: Liquid or solid?
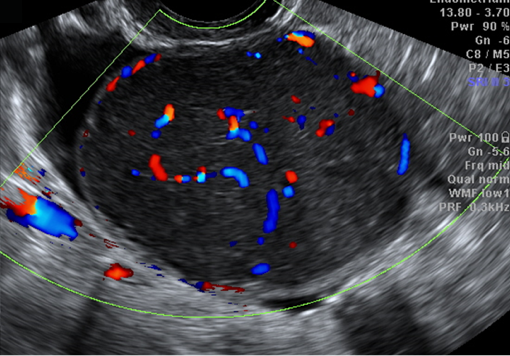
Figure 4b: Liquid or solid?
In the case of Figure 5, hematometry could be suspected at the ultrasound in black and white. However, the presence of multiple internal vessels in the color Doppler establishes the solid nature of the lesion. A Cornier Pipeline Biopsy diagnoses a lymphoma.
Polyp or clot?
In the assessment of uterine bleeding, a focal thickening of the endometrial suggests endometrial lesion (polyp, cancer) or intrcavitary myoma (Leone et al. 2010). However, the presence of a clot must be integrated into the differential diagnosis. Vascularization of the endometrial lesion or myoma is often seen at the Doppler Color examination (Figure 6). Where appropriate, the presence of a clot is excluded.
The absence of a color Doppler signal (Figure 7) suggests the presence of a clot. In the image presented, the straight boundary between the anchogenic liquid on the side of the uterine bottom and the ultrasound structure in the distal part of the cavity also suggests hemorrhagic origin.
Myoma or adenomyosis?
Both myoma and adenomyosis cause the uterine wall to thicken. The myoma is typically well defined and is surrounded by circular vessels, while the adenomiotic lesion is vague and the vessels pass through the lesion without being deviated (Figure 8): translesional vascularization (Van den Bosch et al. 2015).
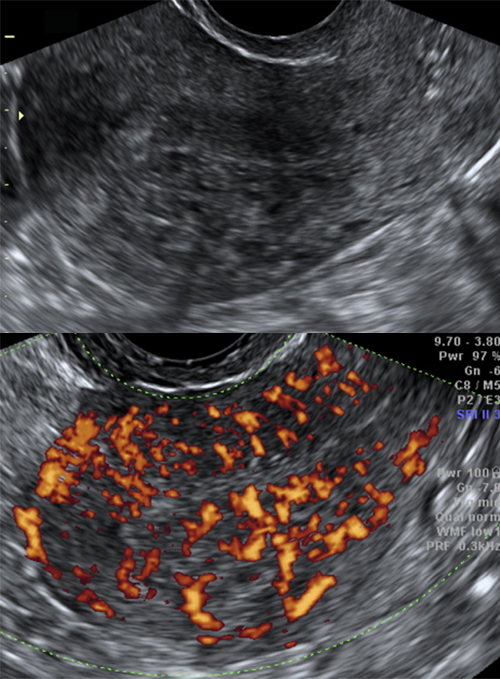
Figure 8: Myoma or adenomyosis?
Hydrosalpinx or vein?
A tubular anechogenic structure attached to the uterus suggests the presence of a hydrosalpinx or a dilated vascular structure. The presence of an intense signal at the color Doppler confirms the second option (Figure 9).
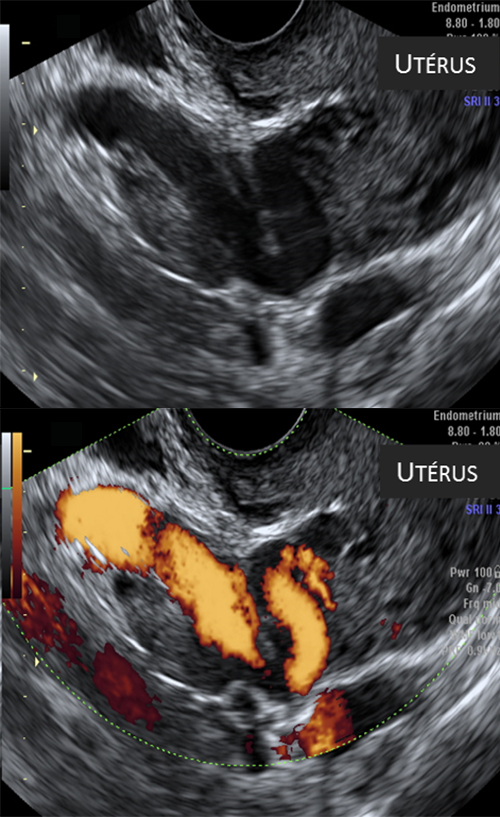
Figure 9: Hydrosalpinx or vein?
Conclusion
- The daily integration of Doppler color into gynecological ultrasound is simple and efficient without extending the examination time.
- The vessel demonstration demonstrates the strength of the lesion and can be useful for differentiating between a benign lesion and a malignant tumor.
References
Click on the references and access the Abstracts on

Epstein E et al. Sonographic characteristics of squamous cell cancer and adenocarcinoma of the uterine cervix. Ultrasound Obstet Gynecol 2010 ; 36 : 512-6. Search the abstractGuerriero S et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: a consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultra Search the abstractLeone FP et al. Terms, definitions and measurements to describe the sonographic features of the endometrium and intrauterine lesions: a consensus opinion from the International Endometrial Tumor Analysis (IETA) group. Ultrasound Obstet Gynecol 2010 ; 35 : Search the abstractTimmerman D et al. ; International Ovarian Tumor Analysis (IOTA) Group. Terms, definitions and measurements to describe the sonographic features of adnexal tumors: a consensus opinion from the International Ovarian Tumor Analysis (IOTA) Group. Ultrasound Search the abstractVan Calster B et al. Practical guidance for applying the ADNEX model from the IOTA group to discriminate between different subtypes of adnexal tumors. Facts Views Vis Obgyn 2015 ; 7 : 32-41. Search the abstractVan den Bosch T et al. Occurrence and outcome of residual trophoblastic tissue: a prospective study. J Ultrasound Med 2008 ; 27 : 357-61. Search the abstractVan den Bosch T et al. Terms, definitions and measurements to describe sonographic features of myometrium and uterine masses: a consensus opinion from the Morphological Uterus Sonographic Assessment (MUSA) group. Ultrasound Obstet Gynecol 2015 ; 46 : 284- Search the abstractVan den Bosch T et al. Color Doppler and gray-scale ultrasound evaluation of the postpartum uterus. Ultrasound Obstet Gynecol 2002 ; 20 : 586-91. Search the abstractVan den Bosch T, Van Schoubroeck D, Timmerman D. Maximum Peak Systolic Velocity and Management of Highly Vascularized Retained Products of Conception. J Ultrasound Med 2015 ; 34 : 1577-82. Search the abstractVan Holsbeke C et al. Endometriomas: their ultrasound characteristics. Ultrasound Obstet Gynecol 2010 ; 35 : 730-40. Search the abstractVangoitsenhoven M, Van den Bosch T. Endometroid carcinoma not to be mistaken for deep infiltrating endometriosis on transvaginal ultrasound. Ultrasound Obstet Gynecol 2017 (in press). Search the abstract