Obstetric imaging
Illustrations of the cranial length (CLA) and nucal clarity (CN) data sheet
This fact sheet is the result of the analysis of recommendations, practices and their improvements in France and internationally.
1) First
The first is abdominal and/or endovaginal. The abdominal track is usually sufficient.
2) Limits
The CLA must be between 45 and 84 mm corresponding to an examination carried out between 11 and 13 weeks and 6 days of amenorrhea.
Nucal clarity measurements made outside these limits are not validated to be included in a trisomy risk calculation 21.
3) Sagittal Position
√ Quality Criteria
The quality criteria for the sagittal cutting are at the level of:
• Cephalic Pole: For the LCC and CN
- Forward: visibility of nose tip (linear ultrasound), rectangular bone palate, ponctiform chin (Figure 1)
- Middle: hypoechogenic diencephalus (Figures 2 and 3)
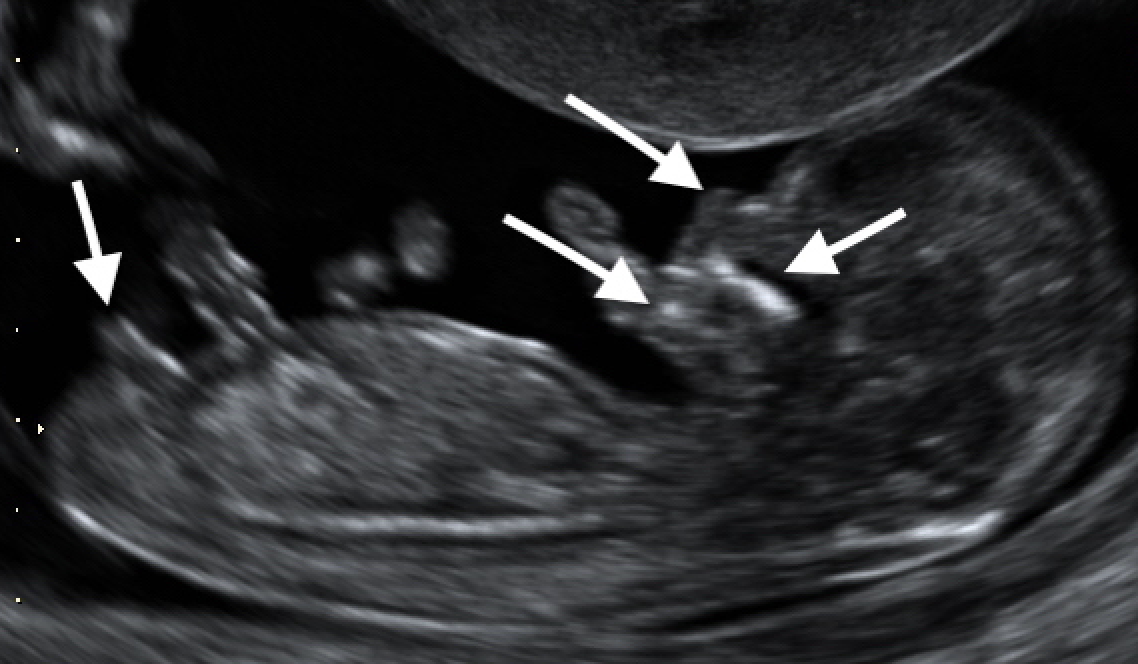
Figure 1: Sagittal position; Forward: visibility of the tip of the nose (linear ultrasound), the bone palate rectangular echogene, the ponctiform chin.

Figure 2: Sagittal position; In the middle: hypoechogenic diencephalus.
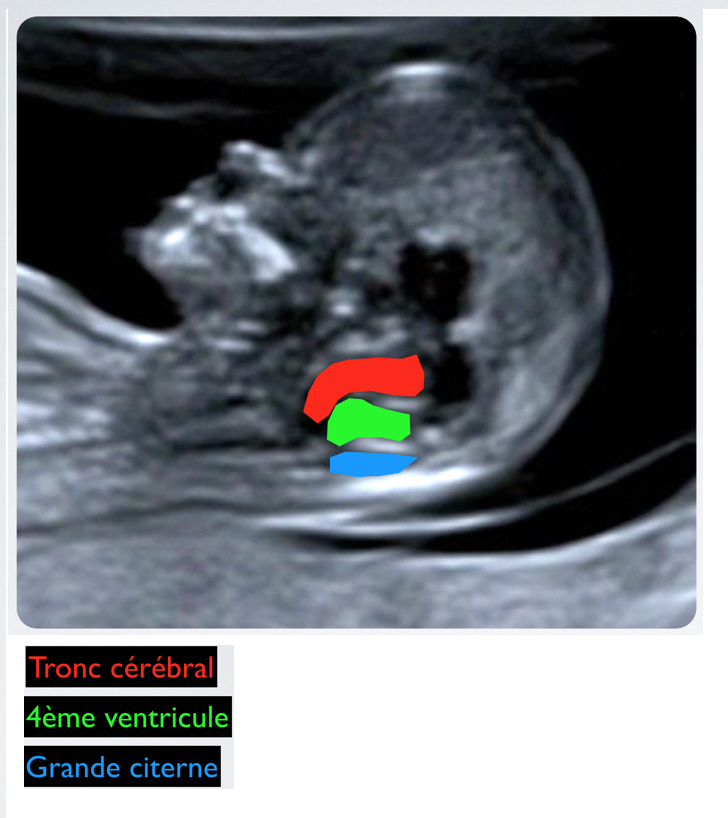
Figure 3: Sagittal position; In the middle: hypoechogenic diencephaly.
• Caudal Pole: For LCC
- Visibility of the genital tuber (Figure 4)

Figure 4: Sagittal Position: visibility of the genital tuber.
√ Notes
For CN : The visualization of the frontal maxillary process as an ultrasonic linear structure perpendicular to the bone palate is accepted. It is linked to an angulation up to 10 degrees of the cutting plane relative to the reference plane. The tip of the nose is no longer visible, but the clean bones of the nose remain so (Figure 5).
An angulation of more than 10° is first translated into a triangular maxillary and then into the visualization of an orbit. The measure of nucal clarity, reduced, cannot be validated under these conditions (Figure 6).
For the CCA : The visualization of an orbit is accepted. Ideally the genital tuber should be visualized but the presence of the proximal part of the thigh is accepted (Figures 7 and 8).
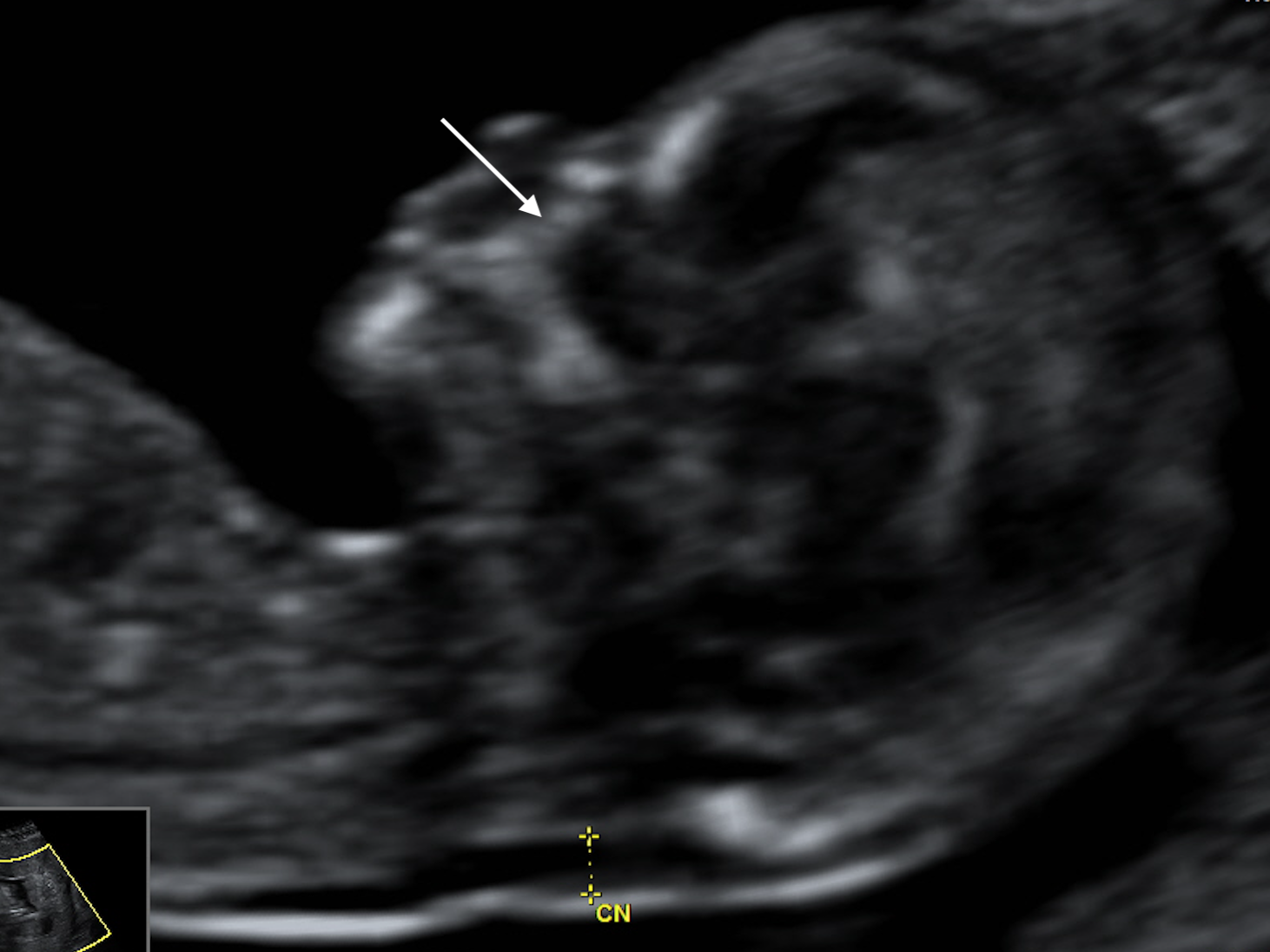
Figure 5: Sagittal position; For CN: visualization of the frontal maxillary process as an ultrasonic linear structure perpendicular to the bone palate is accepted. It is linked to an angulation up to 10 degrees of the cutting plane relative to the reference plane. The tip of the nose is no longer visible, but the clean bones of the nose remain visible.
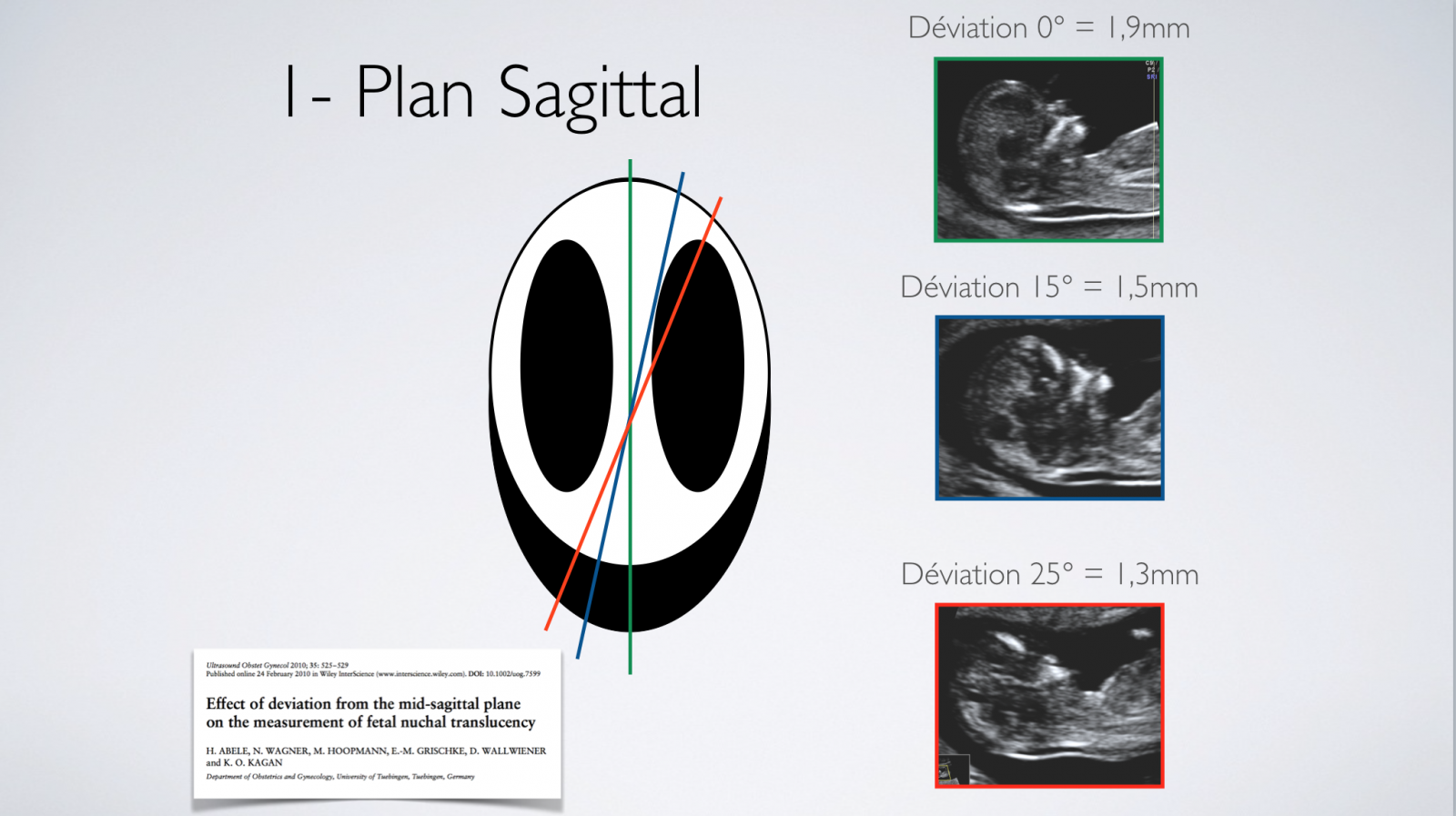
Figure 6: Sagittal position; An angulation of more than 10° results first in a triangular maxillary and then in the visualization of an orbit. The measurement of nucal clarity, reduced, cannot be validated under these conditions.
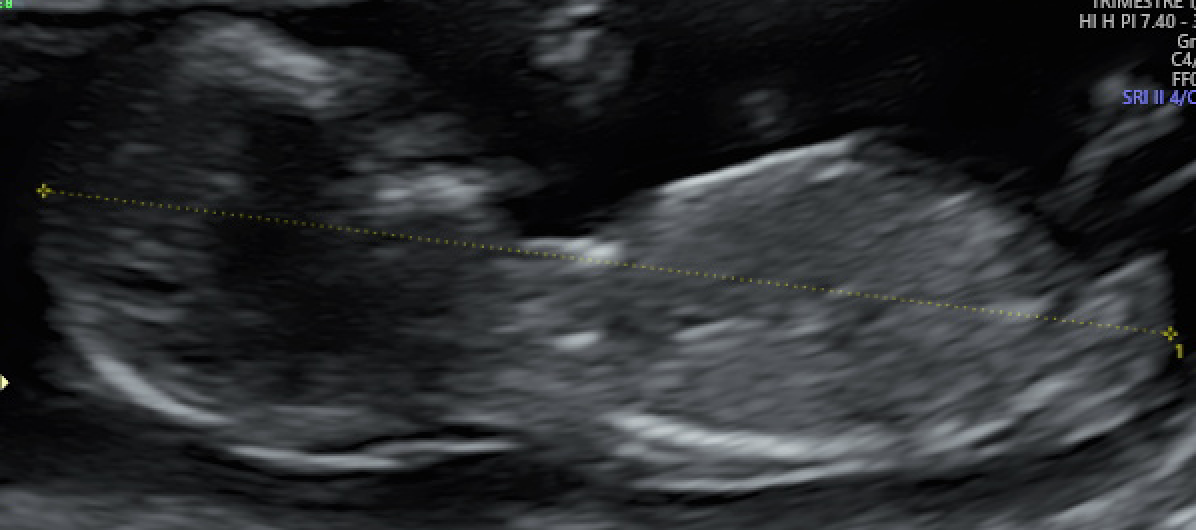
Figure 7: Sagittal position; For the LCC: viewing an orbit is accepted. Ideally the genital tuber should be visualized but the presence of the proximal part of the thigh is accepted.

Figure 8: Sagittal position; For the LCC: viewing an orbit is accepted. Ideally the genital tuber should be visualized but the presence of the proximal part of the thigh is accepted.
4) Area of Interest
√ Quality Criteria
The area of interest to be measured should occupy most of the screen (≥ 75%).
CCA: Head to genital tuber (Figure 9)
CN: Head and thorax (Figure 10)
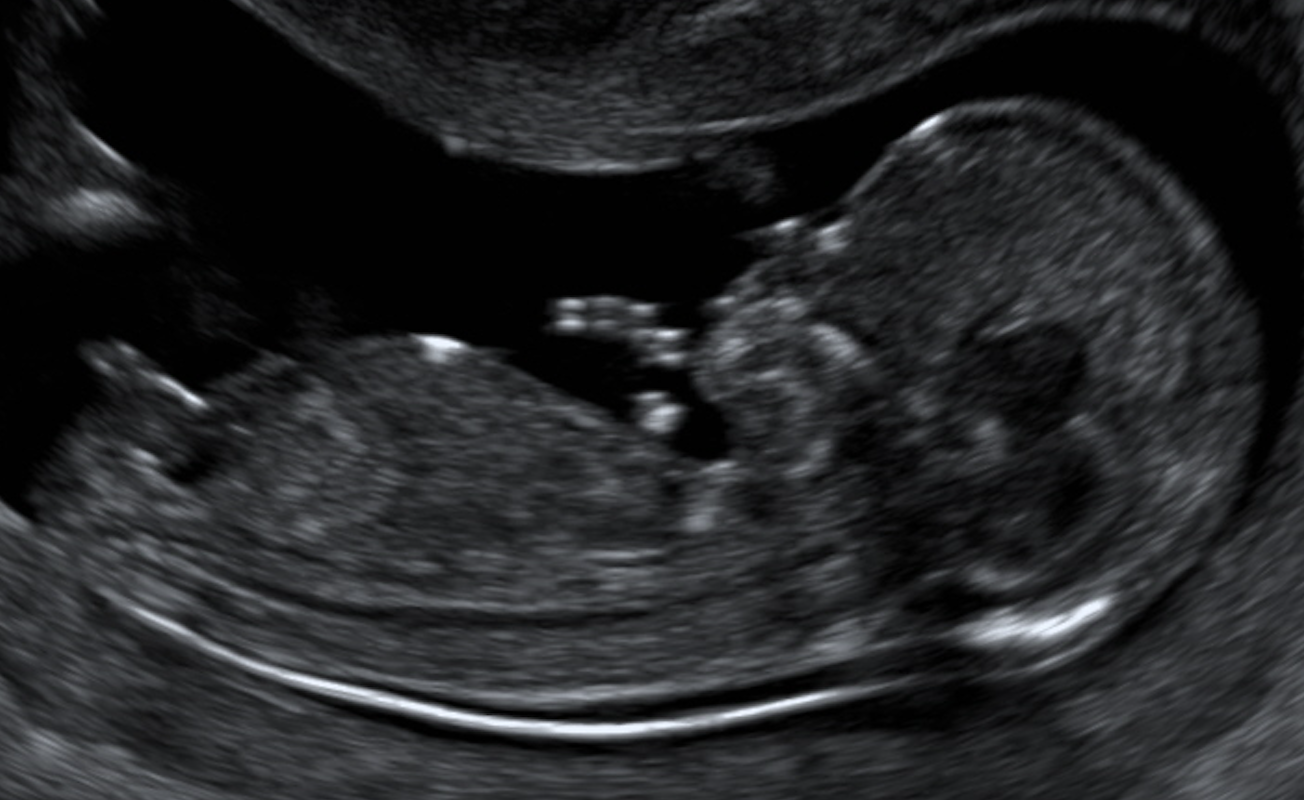
Figure 9: Region of interest; LCC: head to the genital tuber.

Figure 10: Region of interest; CN: head and chest.
√ Notes
Enlargement is essential to optimize cursor positioning (Figure 11).
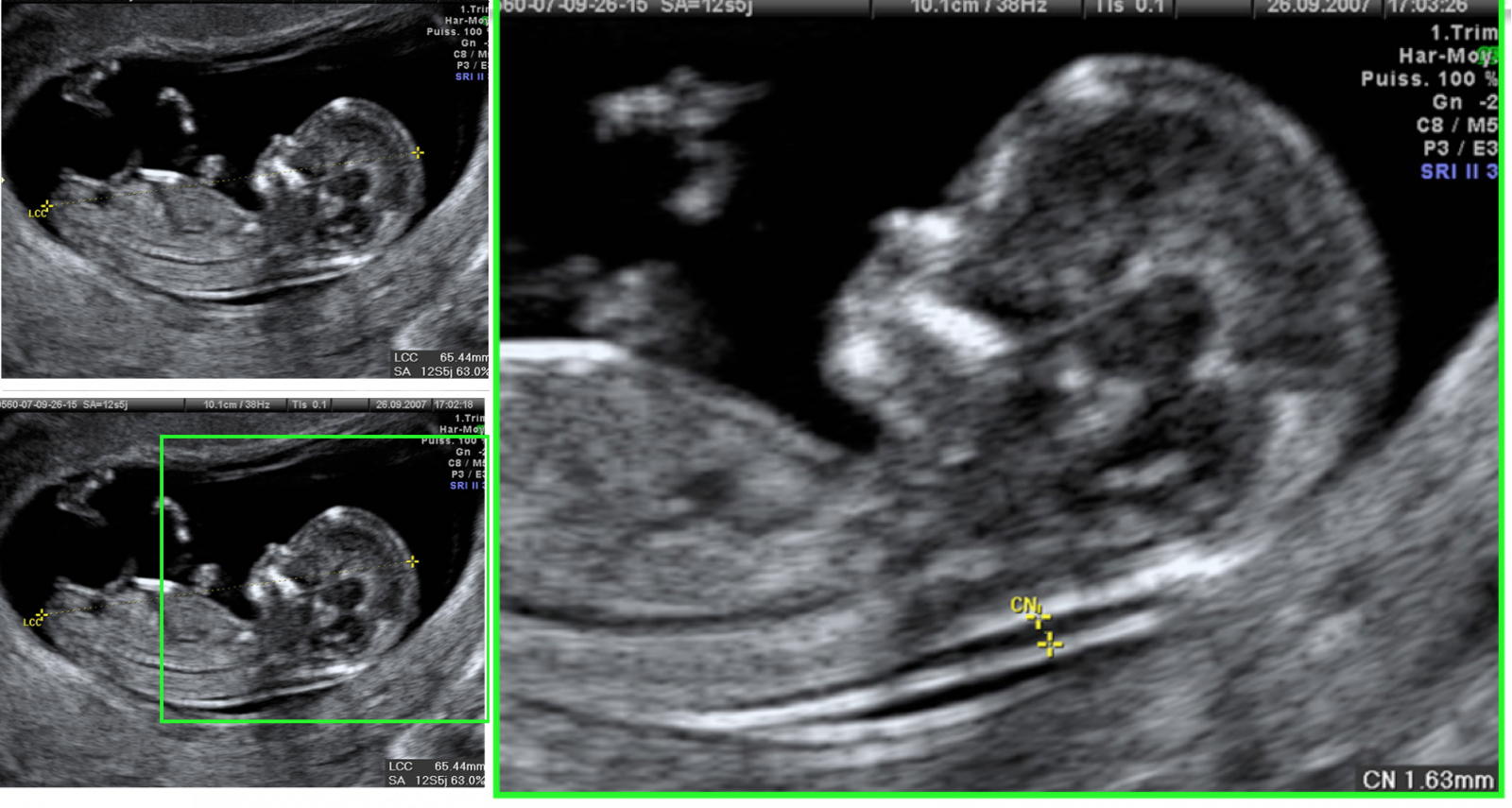
Figure 11: Region of interest; Enlarge is essential to optimize cursor positioning.
5) Cursor Position
√ Quality Criteria
Cursors must be positioned for:
• Cranio-caudal length:
- At the cephalic level: top of the skull vault
- At the caudal level: caudal tip under the genital tuber (Figure 12)
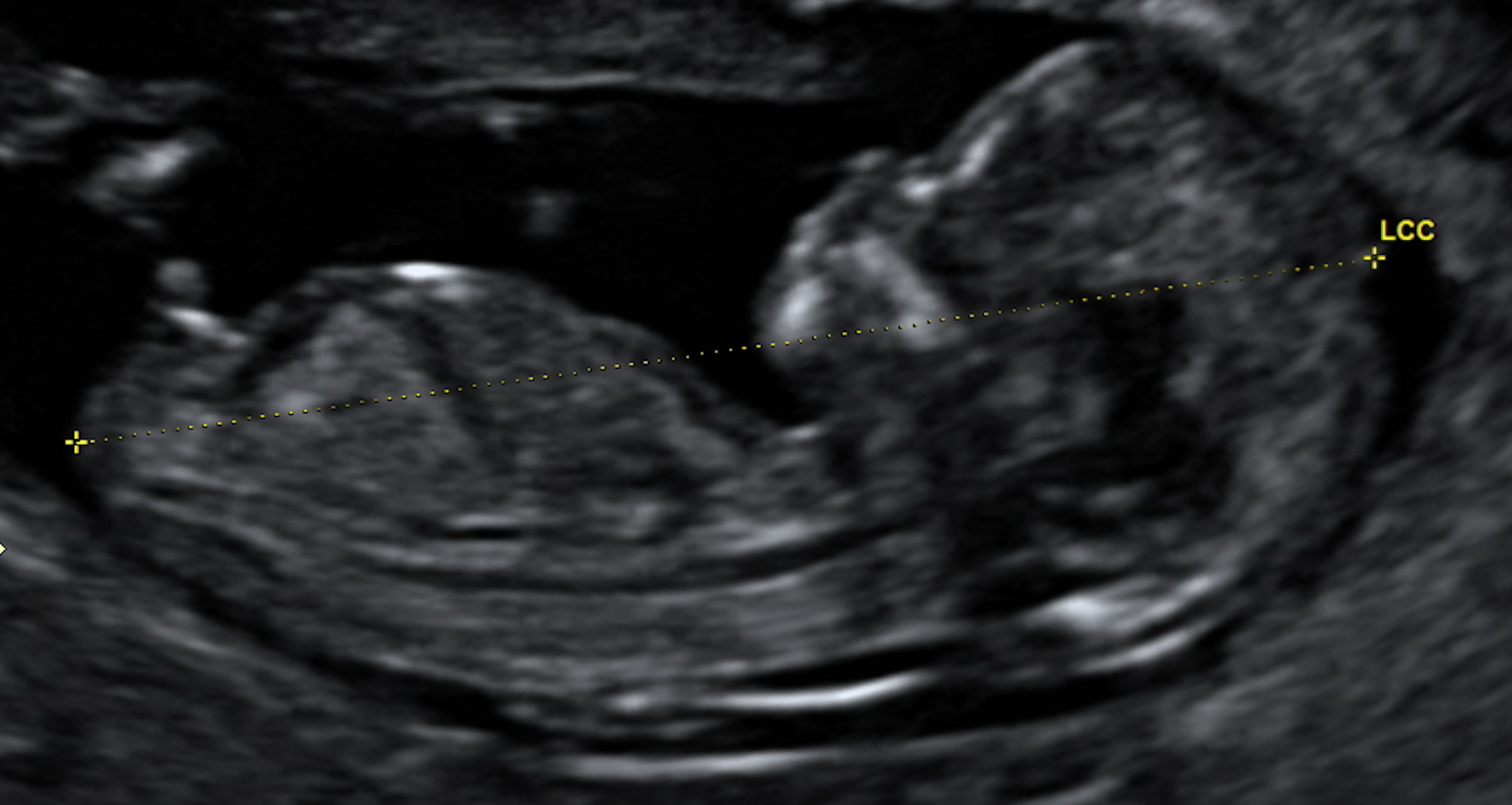
Figure 12: Cursor position Cranial-caudal length. At the cephalic level, the top of the skull arch. At the caudal level, the caudal end under the genital tuber.
• Nucal clarity
- "On to on"
- The horizontal branch of the cross of the slider blends with the edge of nucal clarity
- The measurement is perpendicular to the axis of nucal clarity
- At the level of the greatest thickness
(Figures 13 and 14)

Figure 13: Cursor position. Nucal clarity; The horizontal branch of the cross of the cursor is confused with the edge of nucal clarity - The measurement is perpendicular to the axis of nucal clarity - At the level of the greatest thickness.
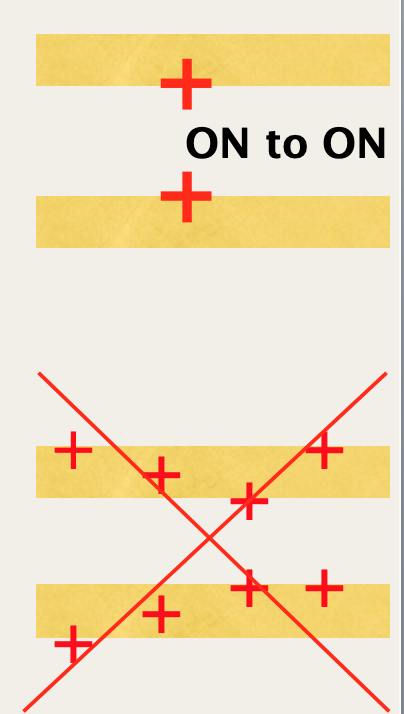
Figure 14: Cursor position. Nucal clarity; "On to On."
√ Notes
• Cranial-caudal length
It requires a good delimitation of the cephalic and caudal ends.
At the cephalic level, the cursor must be placed at the most distal point of the top of the skull.
At the caudal level, the cursor is placed at the most distal point under the genital tuber. If the tuber is masked by the thigh, the measurement is made on the posterior skin edge of the thigh root (Figure 15).
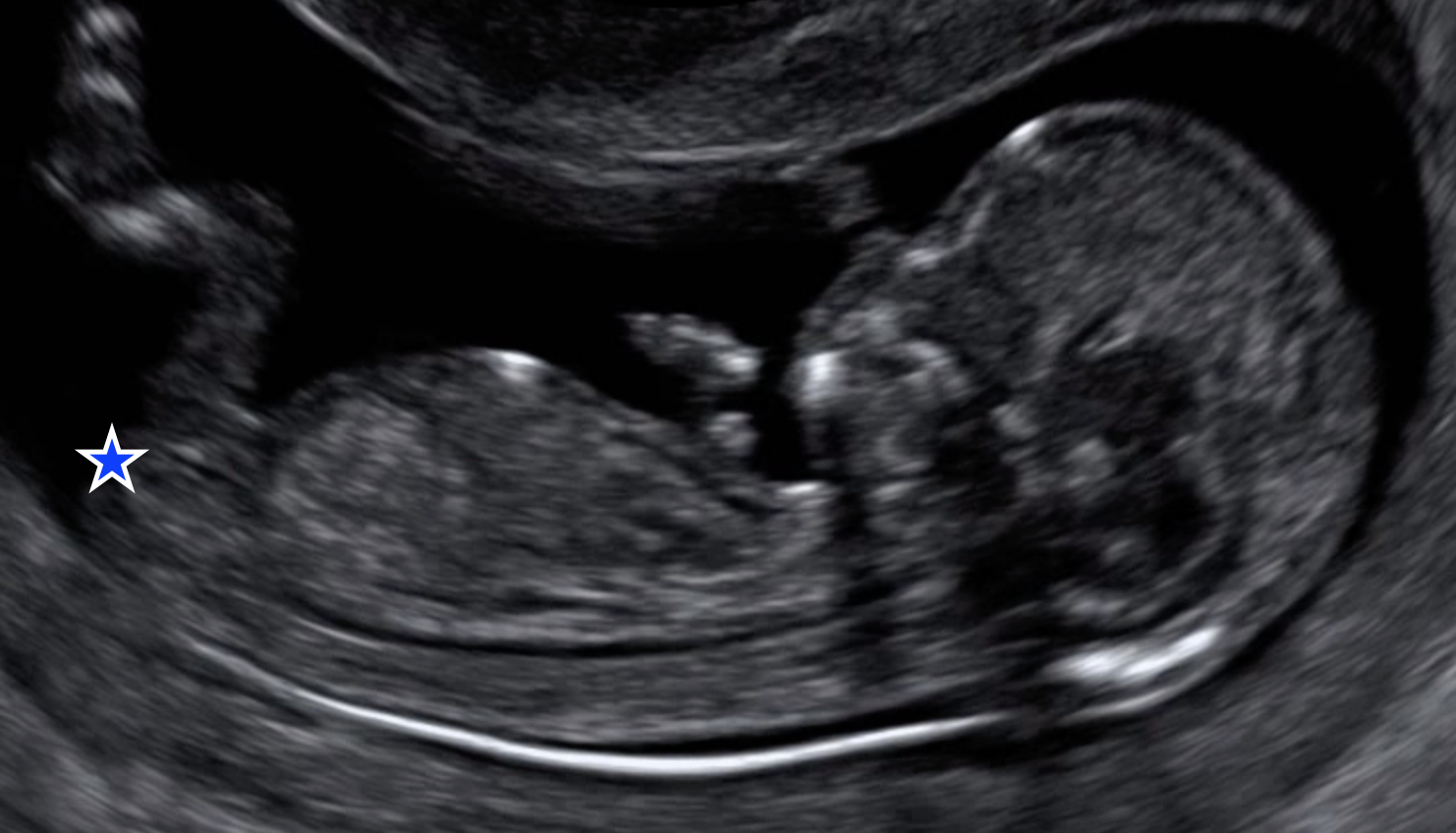
Figure 15: Cursor position. Cranial-caudal length; At the caudal level, the cursor is placed at the most distal point under the genital tuber. If the tuber is hidden by the thigh, the measurement is made on the posterior skin edge of the thigh root.
• Nucal clarity
- The precise delimitation of the nucal clarity requires the most orthogonal first possible by the ultrasonic beam (Figure 16).
- The measurement is cervical and not occipital or dorsal (Figure 17).
- The amnios must be identified and not confused with the skin (Figure 18).
- Several measurements are made and more large (according to quality criteria) is chosen.
- The position of the cord can hinder the measurement: in about 5% of cases, the cord surrounds the neck of the fetus, changing the nucal thickness. The average of the two measurements correctly performed, just above and just below the cord can be used or a further examination carried out later (Figure 19).
- Automatic measurements can be used. It is therefore essential to use the "on to" technique.
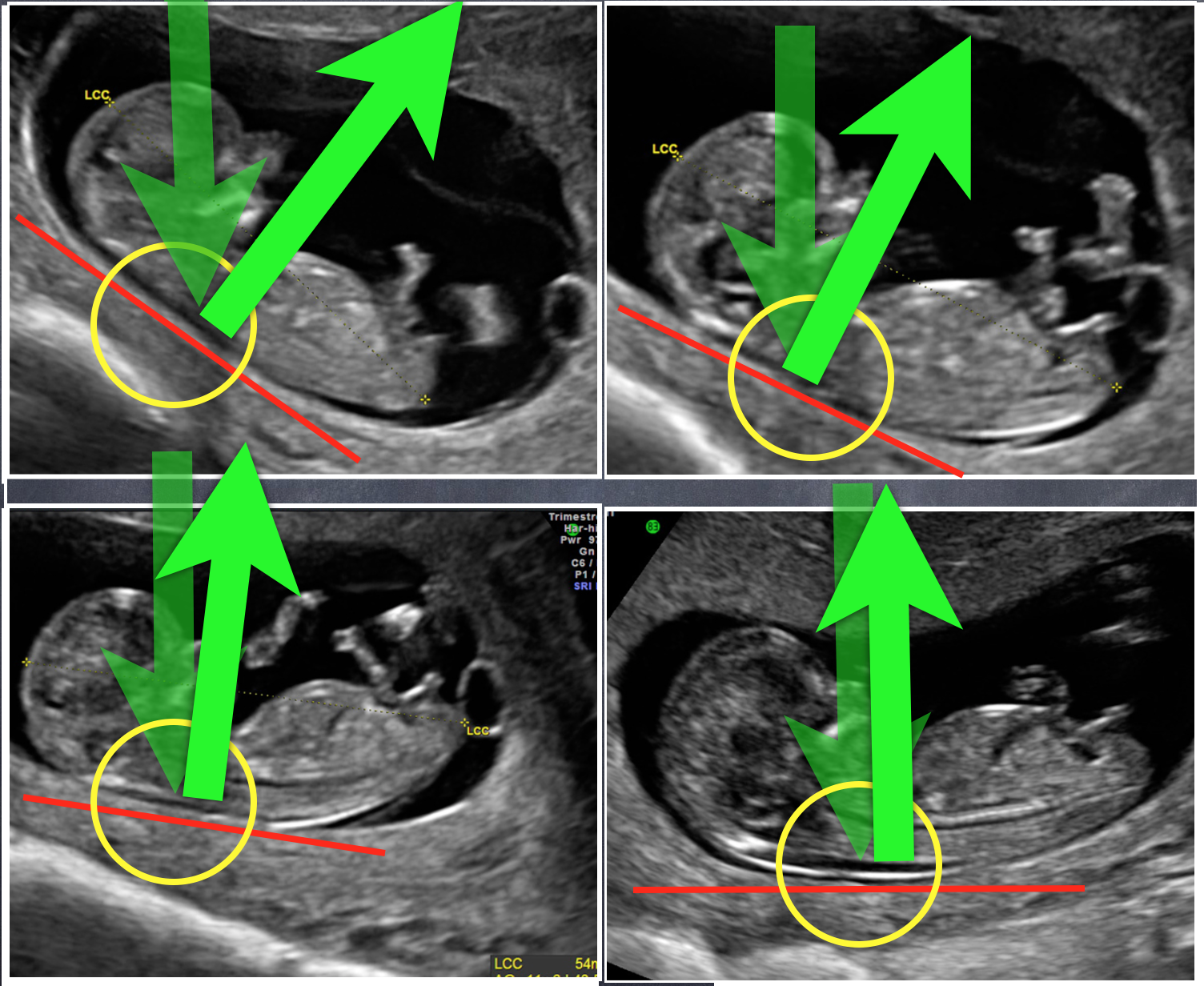
Figure 16: Cursor position. Nucal clarity; The precise delimitation of the nucal clarity requires the most orthogonal first possible by the ultrasonic beam.
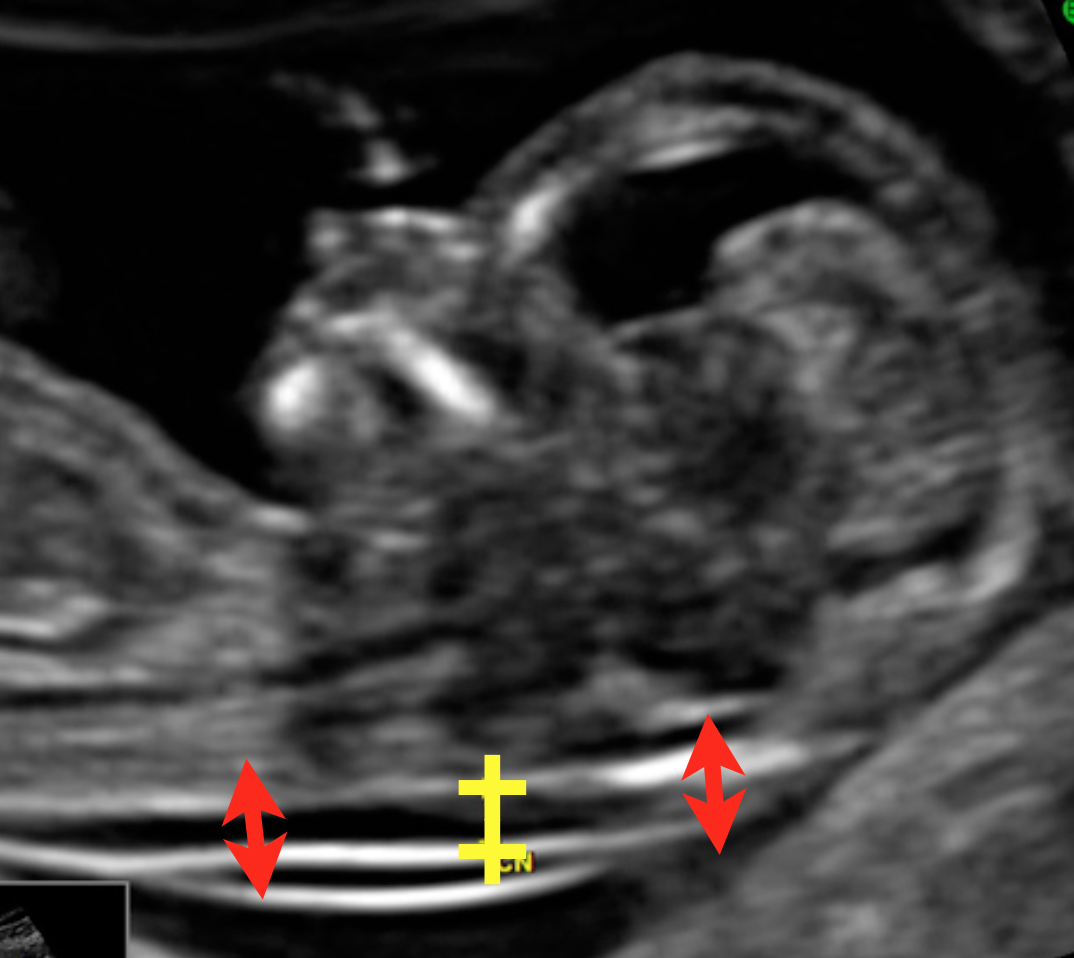
Figure 17: Cursor position. Nucal clarity; The measurement is cervical and not occipital or dorsal.
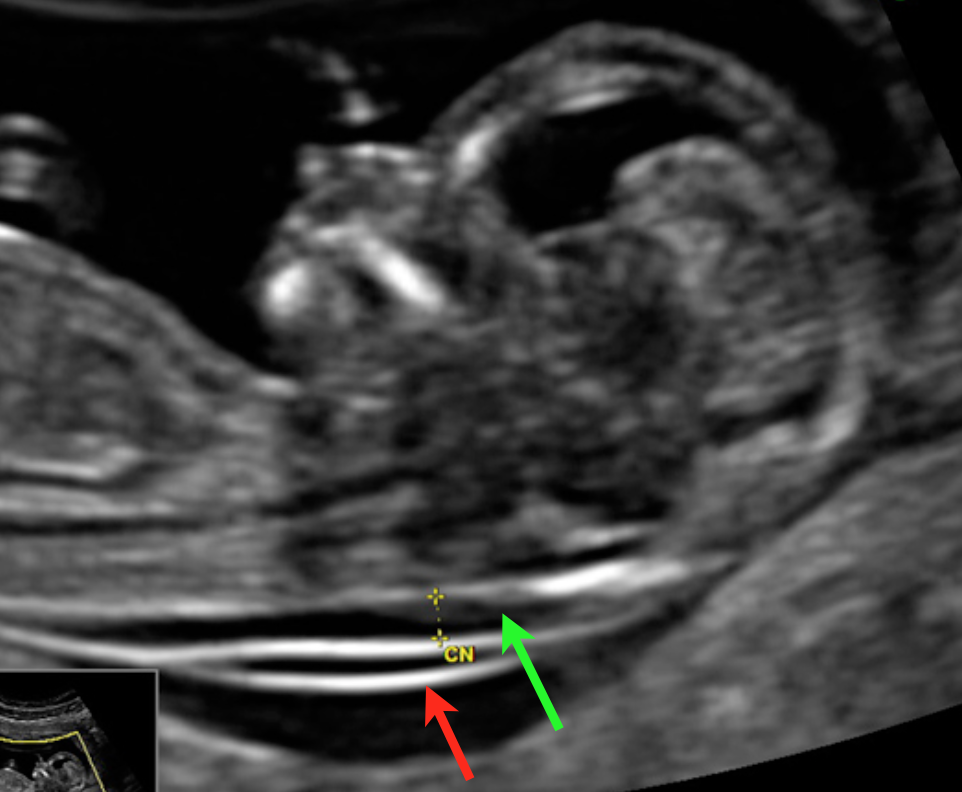
Figure 18: Cursor position. Nucal clarity; The amnios must be identified and not confused with the skin.
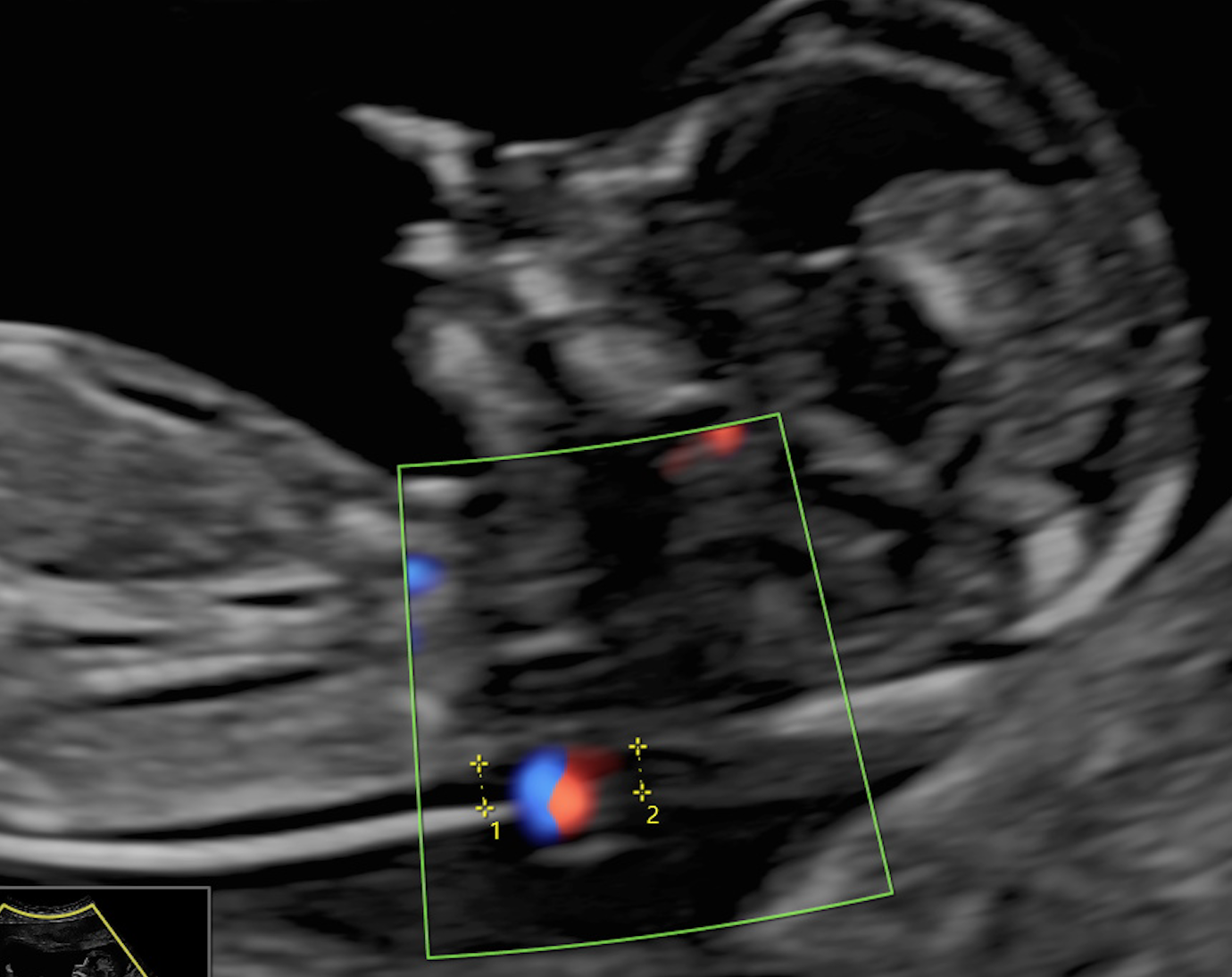
Figure 19: Cursor position. Nucal clarity; The position of the cord can hinder the measurement: in about 5% of cases, the cord surrounds the neck of the fetus, changing the nucal thickness. The average of the two measurements correctly performed, just above and just below the cord can be used or a further examination performed later.
6) Neutral position of the fetal cephalic pole
√ Quality Criteria
The quality criteria for the neutral position of the fetal cephalic pole are:
- The presence of amniotic fluid between the chin and the thorax.
- The absence of flexion or deflection of the cephalic pole.
- The angle between the bone palate and the anterior wall of the neck is close to 90°.
(Figure 20)
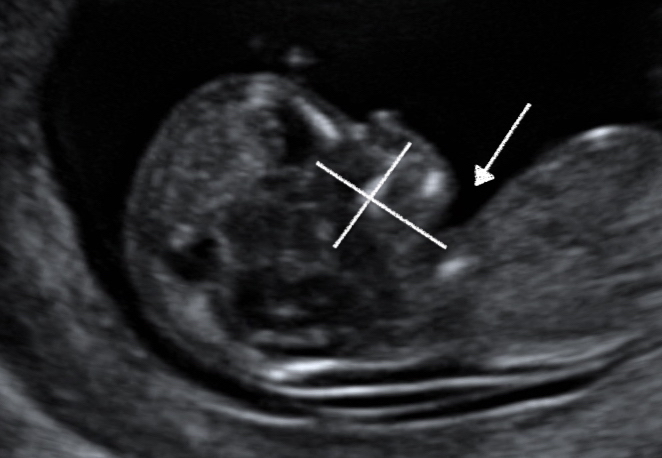
Figure 20: Neutral position of the fetal cephalic pole; The presence of amniotic fluid between chin and chest. The absence of flexion or deflection of the cephalic pole. The angle between the bone palate and the anterior wall of the neck is close to 90°.
√ Notes
The CLA and CN measurements vary if the headpole position is not intermediate.
- Fetal flexion:
There is no amniotic fluid between chin and chest (Figure 21).
This results in a decrease in the CCA and a decrease in CN (Figure 22).
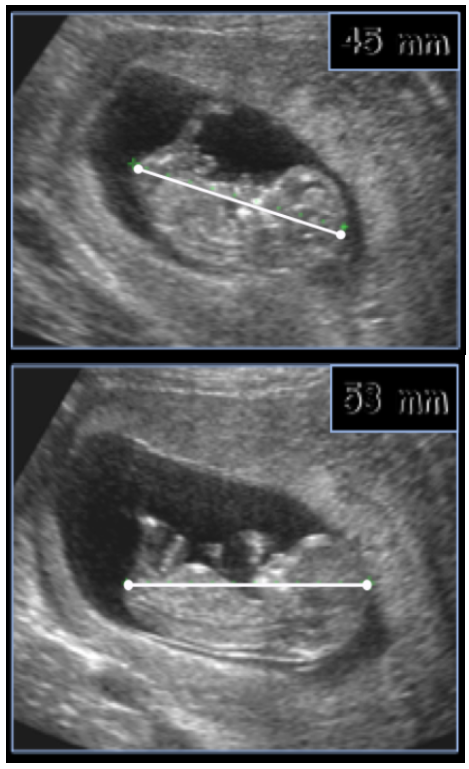
Figure 21: Neutral position of the fetal cephalic pole; There is no amniotic fluid between chin and chest.
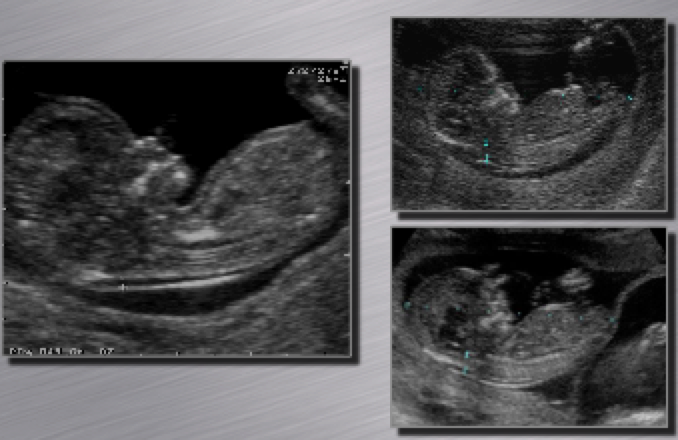
Figure 22: Neutral position of the fetal cephalic pole; The result is a decrease in the CCA and a decrease in CN.
- Fetal extension:
The head is expanding. The angle between the chin and the anterior wall of the neck is greater than 90° (Figure 23), resulting in an increase in the CCA and CN (Figure 24).
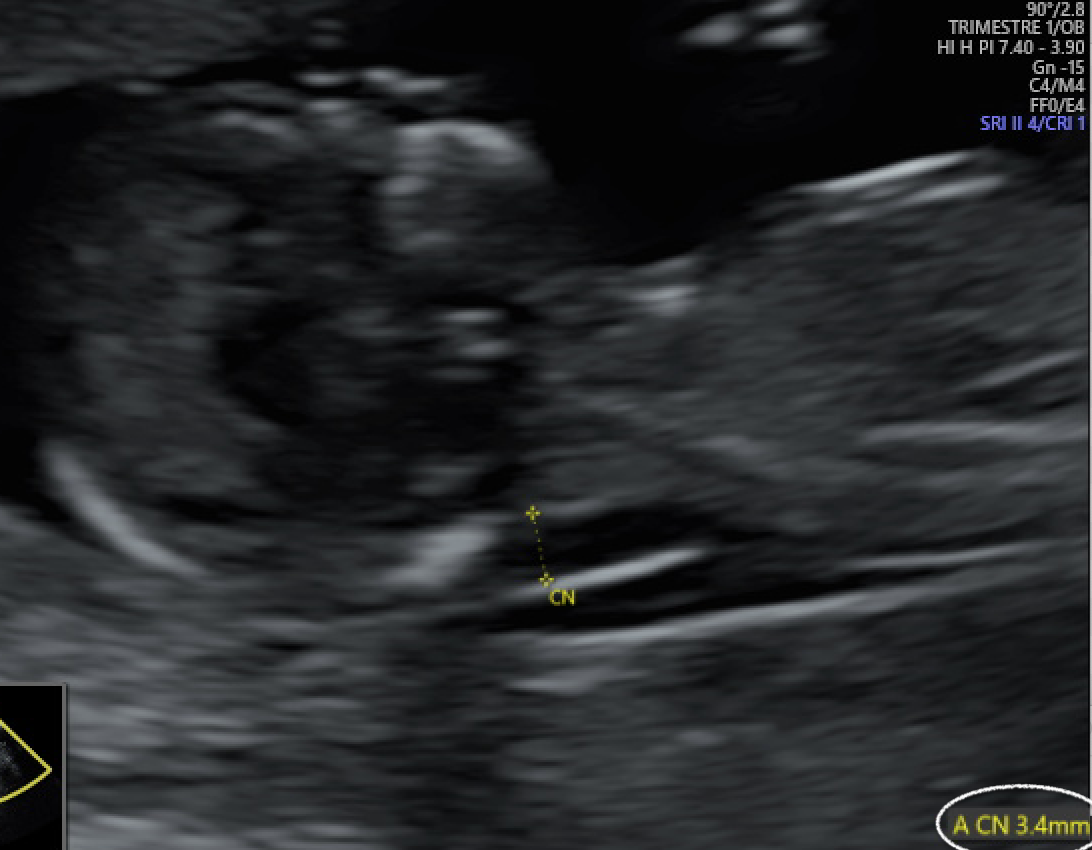
Figure 23: Neutral position of the fetal cephalic pole; The head is expanding. The angle between the chin and the anterior wall of the neck is greater than 90°.
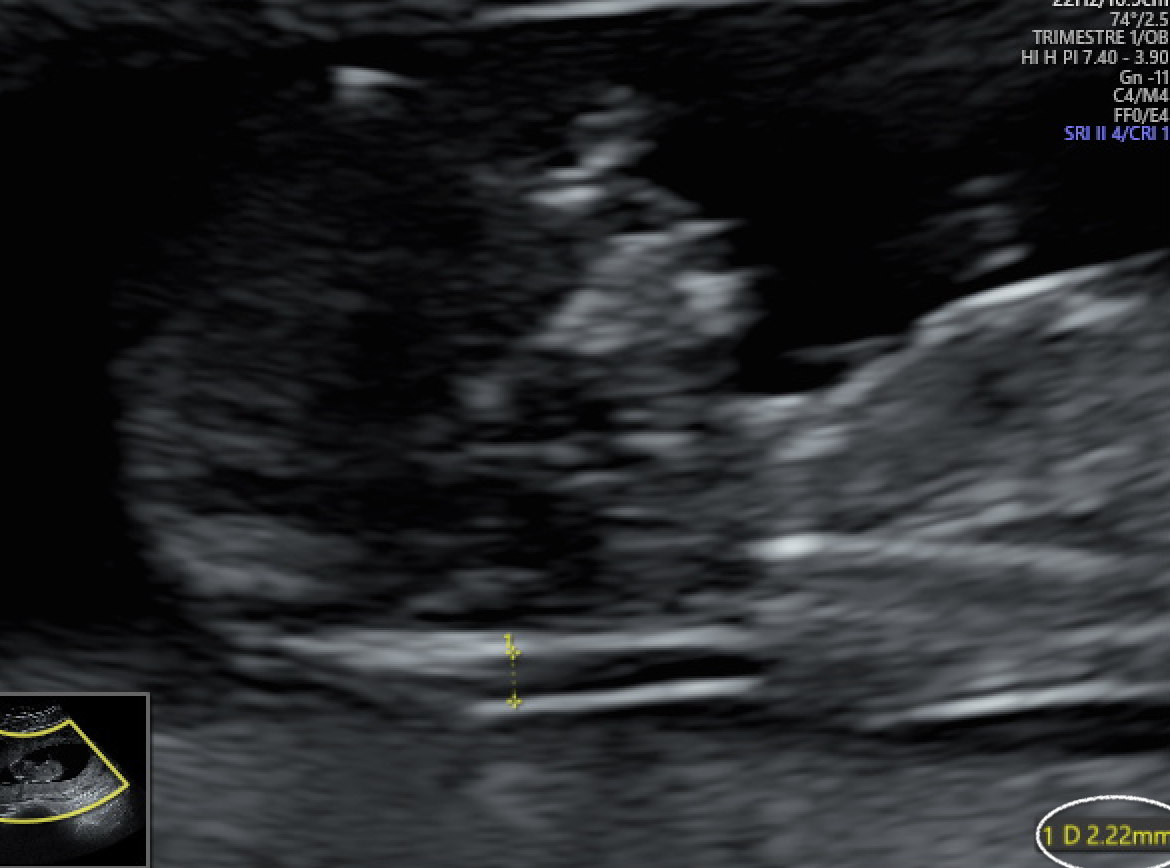
Figure 24: Neutral position of the fetal cephalic pole; The result is an increase in the CCA and CN.
7) Device Settings
Device settings should be optimized:
- Emission power: it must be as low as possible to carry out the examination with the required quality criteria (ALARA principle).
- Image focus: it must be centered on the area of interest in order to avoid a significant degradation of the image and therefore of the markers (Figure 25).
- Gain: it must be kept to a minimum to obtain a good quality image (Figure 26).
- Probe frequency: it must be as high as possible to carry out the examination with the required quality criteria.
- Harmonics: their use depends on the technology used. They should be removed if they cause apparent skin thickening and cervical aponeurosis.
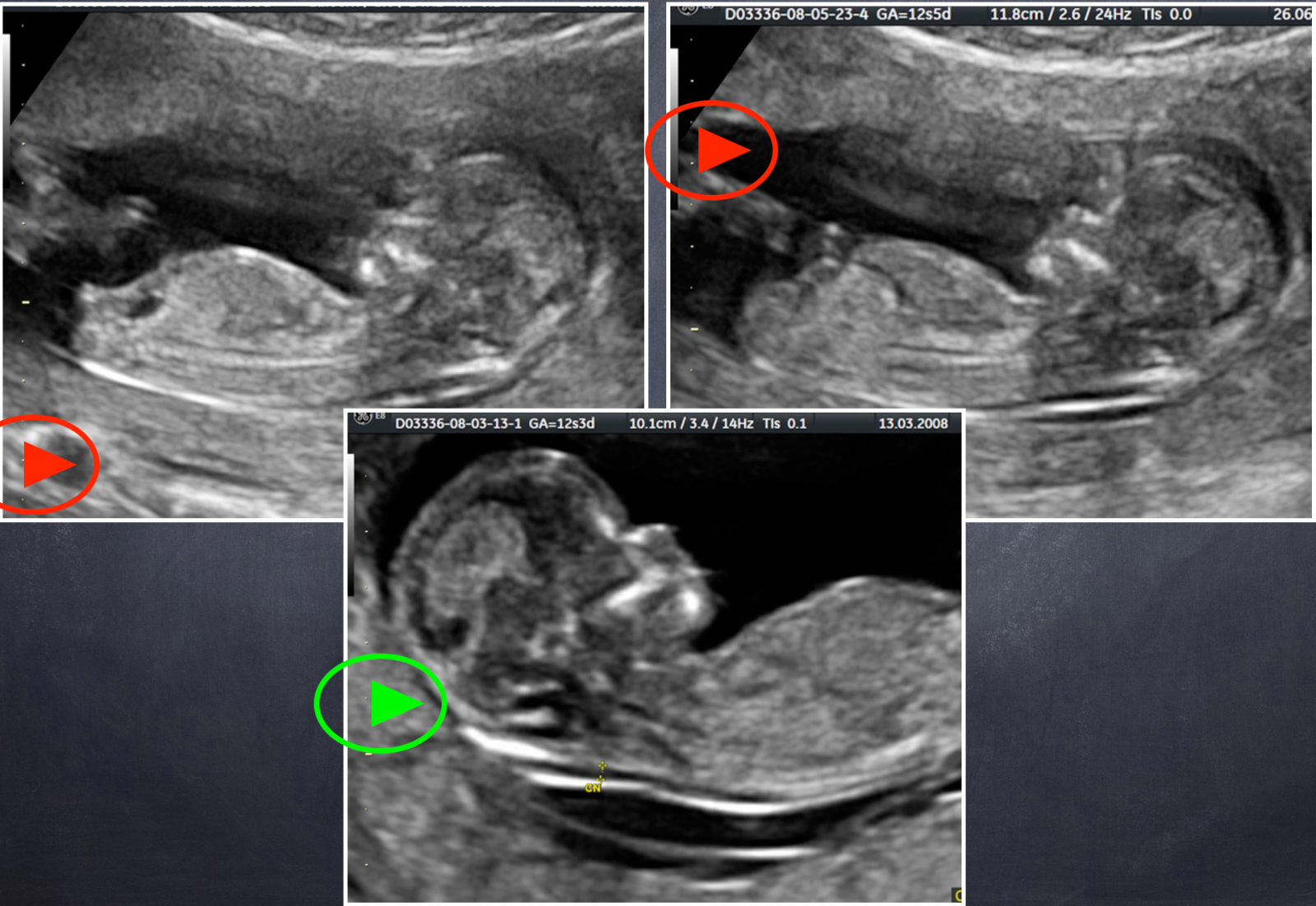
Figure 25: Device settings; Image focus: it must be centered on the area of interest in order to avoid a significant degradation of the image and thus of the markers.
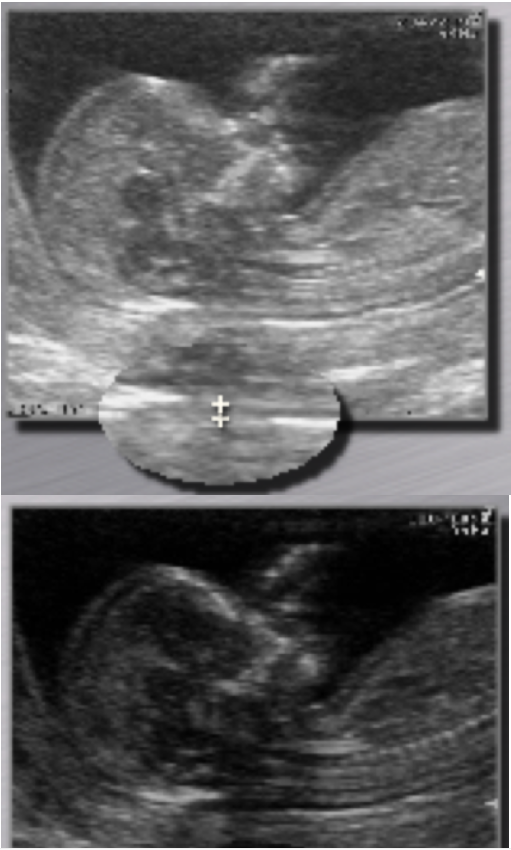
Figure 26: Device settings; Gain: it must be kept to a minimum to obtain a good quality image.
8) 3D, 4D and multiplanar cuts
The quality of the reconstructed images is not currently sufficient to validate the measurements made on these cuts.
References
Click on the references and access the Abstracts on

Nuchal translucency audit : a novel image-scoring method. Herman A, Maymon R, Dreazen E, Caspi E, Bukovsky ; Weinraub Z. Ultrasound Obstet Gynecol.1998 ; 12(6) : 398–403. Search the abstractRapport du Comité National Technique de l’échographie de dépistage prénatal, 2005. Search the abstractQuality control of an image-scoring method for nuchal translucency ultrasonography. N. Fries! ; M. Althuser ; M. Fontanges ; C. Talmant ; PS. Jouk ; M. Tindel ; M. Duyme. Am J Obstet Gynecol, 2007, 272.e1-272.e5. Search the abstractEffect of deviation of nuchal translucency measurements on the performance of screening for trisomy 21. Kagan KO, Wright D, Etchegaray A, Zhou Y, Nicolaides KH. Ultrasound Obstet Gynecol. 2009 ; 33(6) : 657-64. Search the abstractUndermeasurement of nuchal translucencies : implications for screening. Evans MI, Krantz DA, Hallahan TW, Sherwin JE. Obstet Gynecol. 2010 ; 116(4): 815-8. Search the abstractA simple self-assessment tool for the first-trimester ultrasound images. Dhombres F, Friszer S, Bessis R, Jouannic JM. Gynecol Obstet Fertil. 2015 Oct 14. pii:! S1297-9589(15)00265-9. doi: 10.1016/j.gyobfe.2015.09.006. Search the abstract
Articles on the same theme
- 1 of 2
- >