Obstetric imaging
Interest in pelvic MRI in the diagnosis and management of endometriosis
This paper summarizes the interest of MRI in the diagnosis, monitoring and preoperative mapping of endometriosis. Here we discuss the technical elements necessary and sufficient for a precise diagnosis, as well as the semiological elements basic for the proper recognition of the pathology.
Endometriosis is defined by the presence of endometrial tissue outside the endometrial cavity containing both glands and stroma. This disease is common, affecting 10% of women of childbearing age. The average time between the onset of symptomatology and an established diagnosis remains long, close to 8 years. The main symptoms are dysmmenorrhea, dyspareunae and infertility. Endometriosis is now a major public health problem; the Ministry of Health has implemented a national information campaign.
Indications
A pelvic MRI must be preceded by a gynecological ultrasound. It allows a simple and efficient search for endometriomes that appear as cystic formations with a homogeneous thin stab. The search for a deep endometriosis is much more complex and requires an expert ultrasound designer. MRI may be offered in patients with clinical impairment or with an endometriosis visualized in ultrasound (single ovarian or deep endometriosis). It can also be offered in case of negative ultrasound in patients with strong clinical suspicion (dyspareunia or intense dysmmenorrhea).
Techniques
MRI is a well-tolerated and non-invasive test. Significant claustrophobia remains an obstacle. A 4 hour fast is necessary. Rectal washing 2 h prior to examination is routinely required to allow for effective analysis of the double-sigmoidal wall. The realization of rectal or vaginal opacification with ultrasound gel has not shown its superiority in terms of diagnostic performance; it is therefore not recommended to do so. Intravenous injection of gadolinium also showed no superiority(1). Only a subcutaneous injection of glucagon type antiperistaltic is performed 10 minutes before the examination. The analysis is based on T2 sequences without fat saturation. Recent studies have shown the value of the new T2 3D sequences allowing reformatting in all planes of space(2). T1 sequences without and with fat saturation allow the search and characterization of hemorrhagic implants (endometriomes and superficial implants). The interpretation must be performed by an expert radiologist.
Ovarian endometriosis
Endometrioma is a common localization of endometriosis, and can be easily identified by MRI on T1 sequences. They appear in a high-fat T1 signal over the T1 sequence without fat saturation (Figure 1a); this hypersignal persists after the removal of greasy signal (figure 1b). In T2, endometrioma is characterized by a "shading" i.e. a variable signal drop, which can range from a discrete hyposignal T2 to a complete signal vacuum (Figure 1c). Endometrioms are often bilateral and multiple. Tubal damage will be characterized by endometriolic haematsalpinx, which are tubed formations with signal characteristics similar to endometrioma. Differentiation between endometriomes and hematosalpinx is often difficult but essential in LDC care. The MRI allows optimal measurement of these endometriomes and an assessment of residual ovarian function. It will help to detect possible complications of endometrioma: degeneration and overinfection.
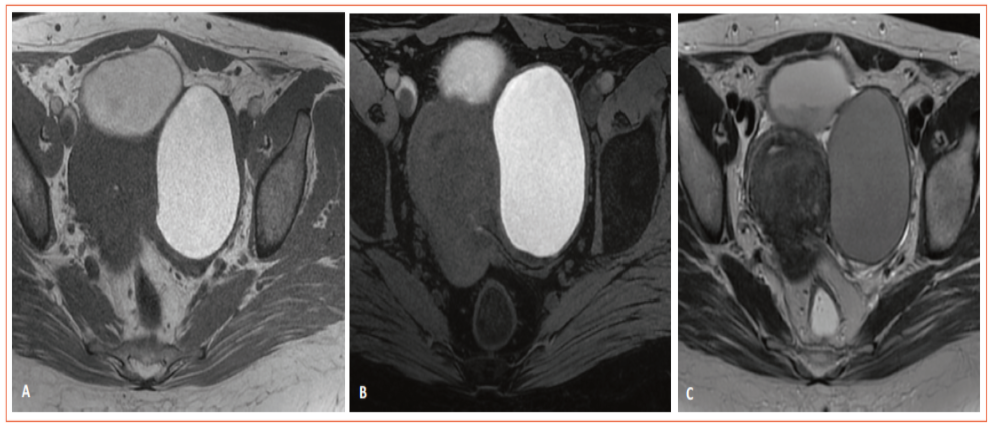
Figure 1: Typical aspect of left ovarian endometrioma. A. Spontaneous T1 hypersignal superior to fat. B. Persistence of T1 hypersignal after fat saturation. C. Moderate T2 hypothesis in relation to a "shading".
• Degeneration will be reported on the presence of a tissue porion appearing in hyposignal T1, intermediate T2 signal, diffusion hypersignal and enhanced after injection. Frequent histological forms are endometrioid epithelial lesions or clear-cell lesions.
• Overinfection of endometriomes will be sought in an obvious infectious context: abscesses will lose their endometriotic signal, have a moderate T1 hypersignal, a peripheral T2 hyposignal and an extremely important parietal enhancement (Figure 2). MRI allows optimal mapping and planning of surgical or radiological drainage.
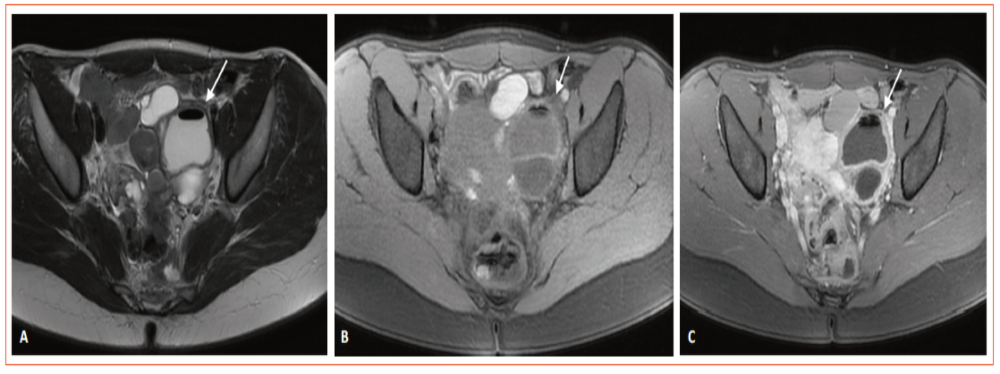
Figure 2: Appearance of overinfection of left ovarian endometrioma. A. Hypogenic T1 with the presence of an open air bubble. B. Hyposignal T2 device of the abscess hull. C. Intense reinforcement after injection of the abscess hull.
Subperitoneural subperitoneal endometriosis
The MRI is very effective in detecting and accurately mapping deep endometriosis lesions. It is characterized by the presence of retractile fibrosis which manifests itself by a hyposignal franc T2 and T1. The presence of T1 FAT SAT hypersignal spots corresponds to overadded surface endometriosis hemorrhagic implants. The most common localization is on uterosacred ligaments and uterinum torus. These anatomical structures are means of binding the uterus to the pelvic wall. The uterosacred ligaments join the sacrorectogenito-pubic blades to their distal porions. The uterinum torus corresponds to the junction of these two ligaments in the back of the isthmus/cervix junction. However, the location of the torus varies in height. In normal conditions, these structures can be visualized; they appear as two linear and fine T2 hyposignal structures. Their visualization is facilitated by the presence of a free spinning in Douglas’s cul-de-sac. An attack will be confirmed by focal thickening greater than 3 mm thick, the presence of spicules or hemorrhagic implants. The search for this is facilitated by the creation of a specific T2 sequence in fine sections at a high resolution of 3 mm thickness parallel to the plane of these ligaments(3). Sensitivity and specificity were estimated at 84 and 89%, respectively, higher than endo-vaginal ultrasound and rectal endoscopy(4). The classical aspect is that of "retro-cervical mustache" with the visualization, just behind the neck, of a spicular thickening of the torus and the origin of the two utero-sacred ligaments (Figure 3).
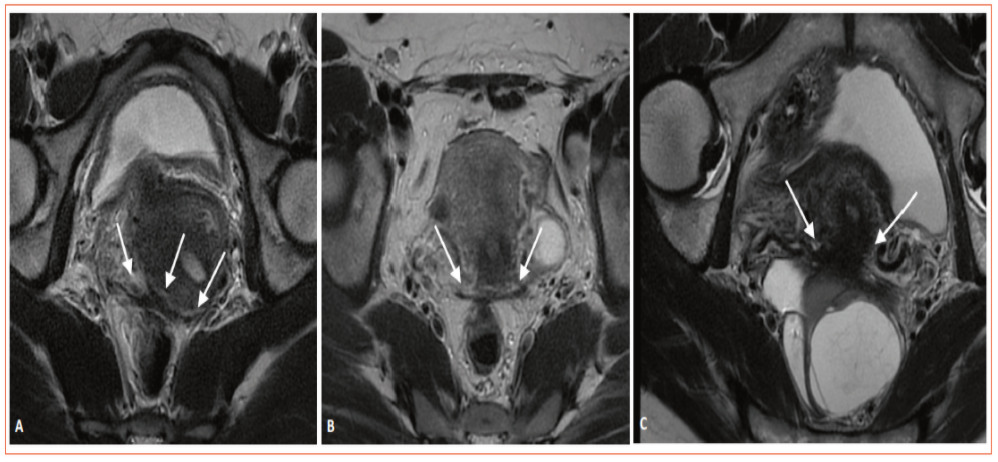
Figure 3: Examples of thickening of the torus and uterosacred ligaments in 3 different patients (white arrows).
This fibrosing attack is frequently accompanied by a retractile phenomenon with the attraction of the ovaries back and the phenomenon of "kissing ovaries" (Figure 4d). The damage will potentially extend back and towards the Sigmodian hinge. Different types of damage are possible, ranging from simple adhesion to damage to the digestive muscular, or even the submucosa.
Digestive impairment will be confirmed in MRI by the presence of free hyposignal nodule T2 in the digestive musculosa. Sensitivity and specificity are estimated at 87% and 93%(4) respectively; in the literature, these performances are lower than those of endovaginal ultrasound and equivalent to those of rectal endoscopy (figure 4). The preparation of a washout, prior to MRI, allows better analysis of the digestive wall. The use of 3D sequences allows a good evaluation and representation in the space of these attacks. The radiological report shall indicate whether this digestive tract is present, the distance between the lower pole of the lesion and the anal margin, the length and thickness of the damage. New discoid surgical resection techniques require an assessment of the attack in the axial plane of the recto-sigmoid, which should not extend over more than 25% of the recto-sigmoidal circumference. The MRI also detects multifocal double-sigmoidal lesions, especially in the case of dolichosigmoid with a second attack next to the left ovarian dip.
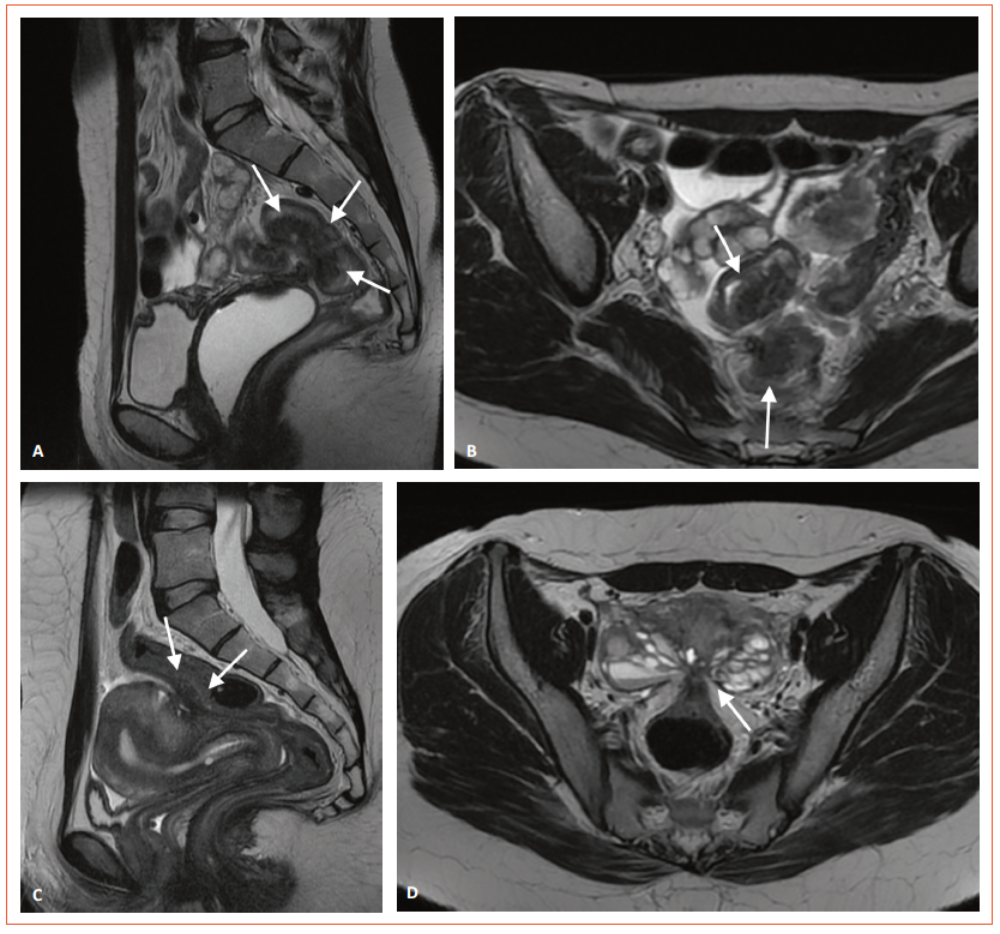
Figure 4: T2 digestive damage in two different patients. A. Extensive damage in T2 sagittal sections with reaching up to the submucosa (white arrows). B. Extensive damage in T2 axial sections with reaching up to the undermucosa (white arrows). C. Limited injury to the T2 hyposignal musculature in T2 sagittal sections (white arrows). D. Restricted to the T2 hyposignal musculature in T2 axial sections (white arrows) with appearance of "kissing ovaries".
The damage can also extend downward by reaching the later vaginal cul-de-sac; his imaging identification is difficult, while his clinical assessment is easy. In MRI, this attack will be characterized by thickening of the posterior vaginal cul-de-sac in hyposignal T2 (Figure 5a and c) and by the presence of hemorrhagic spots in hypersignal T1 after fat saturation (Figure 5b and d). Sensitivity and specificity are estimated at 85% and 72%, much higher than endo-vaginal ultrasound and rectal endoscopy(4). All of these lesions can be associated and perform a complete symphysis of the Douglas-fir with a complete attachment of the sigmoid to the posterior face of the uterus (Figure 4d).
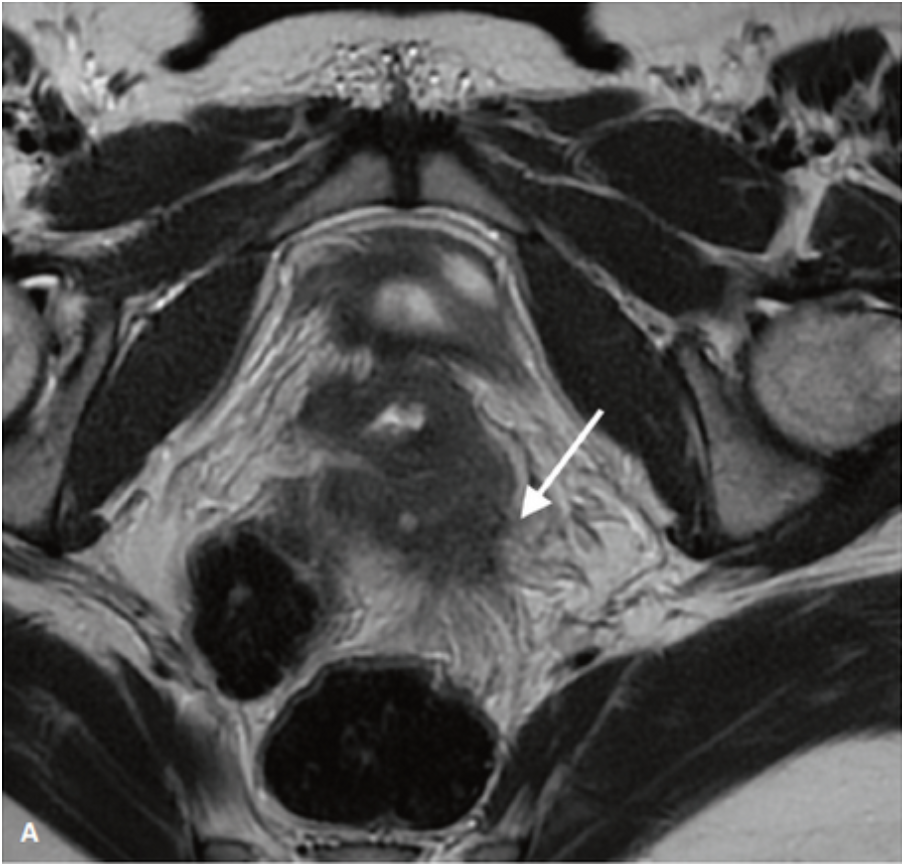

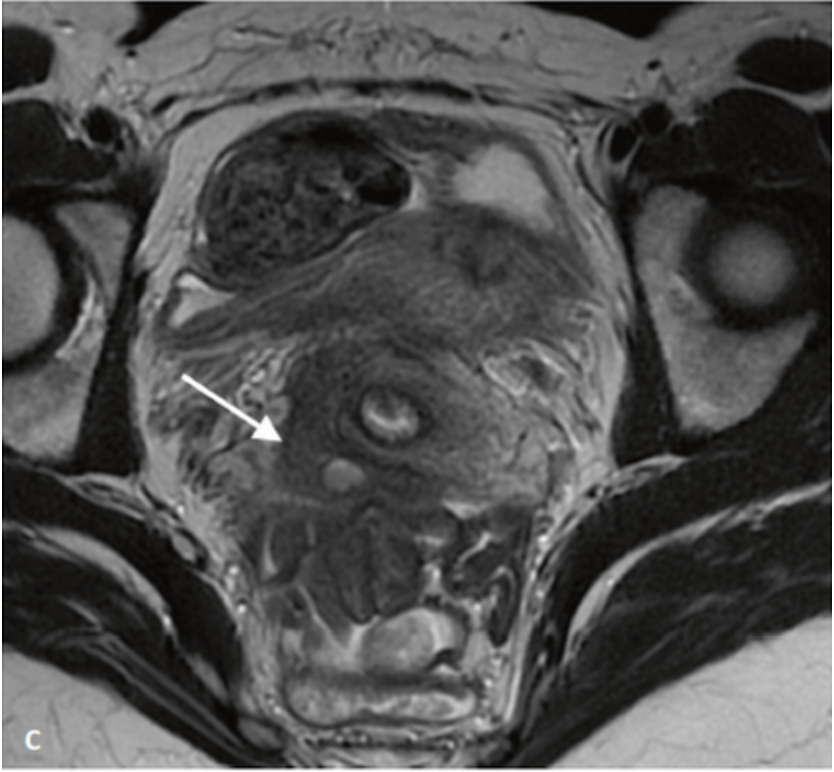

Figure 5: Examples of hindquarters vaginal ascent. A. Spicular damage of the posterior vaginal cul-de-sac in T2 fine cuts (white arrow). B. Hemorrhagic implant visible in T1 sagittals after saturation of the fat next to the posterior vaginal cul-de-sac (white arrow). C. Cystic attack of the posterior vaginal cul-de-sac in T2 fine cuts (white arrow). D. Hemorrhagic implant visible in T1 sagittals after saturation of the fat next to the posterior vaginal cul-de-sac (white arrow).
Anterior subperitoneal endometriosis
Previous localizations are more rare (5-10%), defined by a vesico-uterine cul-de-sac infiltration with a more or less significant damage to the bladder wall. They will be confirmed by the presence of T2 hyposignal nodules in this wall (Figure 6a and b). Past attacks are frequently the seat of hypersignal hemorrhagic implants T1 (Figure 6c). The size and degree of infiltration of the bladder wall should be well described in order to plan an appropriate surgical procedure.
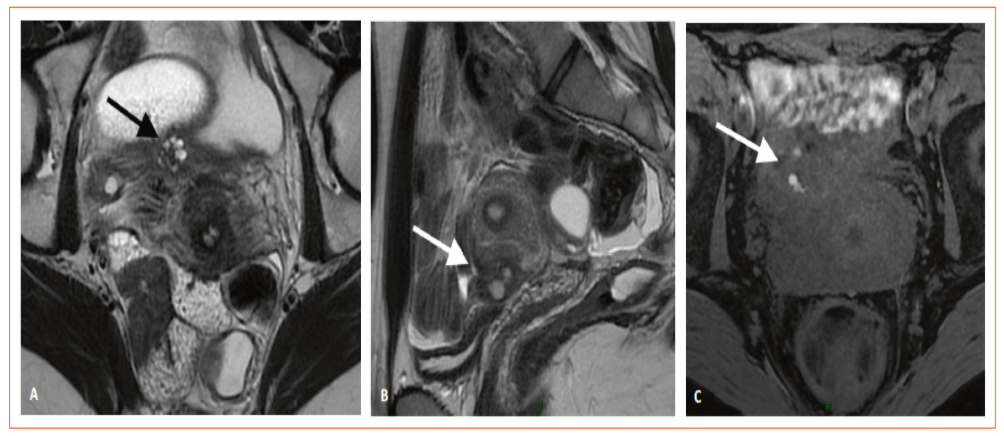
Figure 6: Stroke centered on the vesico-uterine cul-de-sac. A. Spicular nodule centered on the vesico-uterine cul-de-sac in T2 axial sections (black arrow). B. Spicular nodule centered on the vesico-uterine cul-de-sac in T2 sagittal sections (white arrow). C. Hemorrhagic nodule with T1 hypersignal implants with fat saturation (white arrow).
Side endometriosis
Extensive endometriosis attacks will extend to lateral pelvic parameters and walls. These lateral attacks will frequently be complicated by uteral lesions, which may lead to dilation of the pyellocalicial cavities(5). For this reason, any MRI should include kidney exploration. The lesions can also reach the insertion of round ligaments on uterine horns and extend to the Nuck canal by these ligaments (Figure 7).
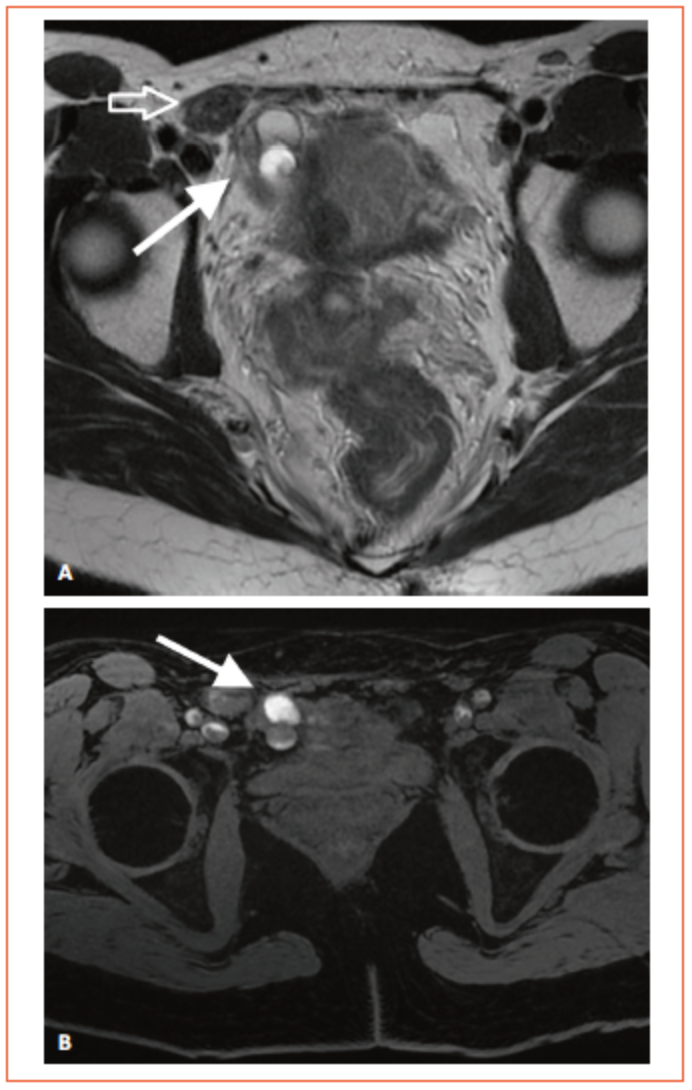
Figure 7: Anterolateral damage centered on the right round ligament extending to the Nuck canal. A. T2 axial cut showing a nodule next to the insertion of the round ligament on the right uterine horn (white arrow) and a hyposignal nodule T2 next to the Nuck canal in the abdominal wall (hollow arrow). B. T1 hemorrhagic implants with saturation of the fat next to the uterine horn (white arrow).
Rare forms
Other rare and more difficult-to-explore diseases may benefit from MRI, such as the reach of the cæ bottom and the last ileal cove (Figure 8). Reaching the anterior abdominal wall may give aspects of pseudo-tumor of the soft parts with masses spelled in hyposignal franc T2 that may be the seat of hemorrhagic implants. Diaphragmatic impairment will only be sought in the case of catamenal pain of the right hypochondre or in the case of a history of catamenal pneumothorax. The visualization of diaphragmatic hemorrhagic implants makes it possible to confirm the diagnosis.
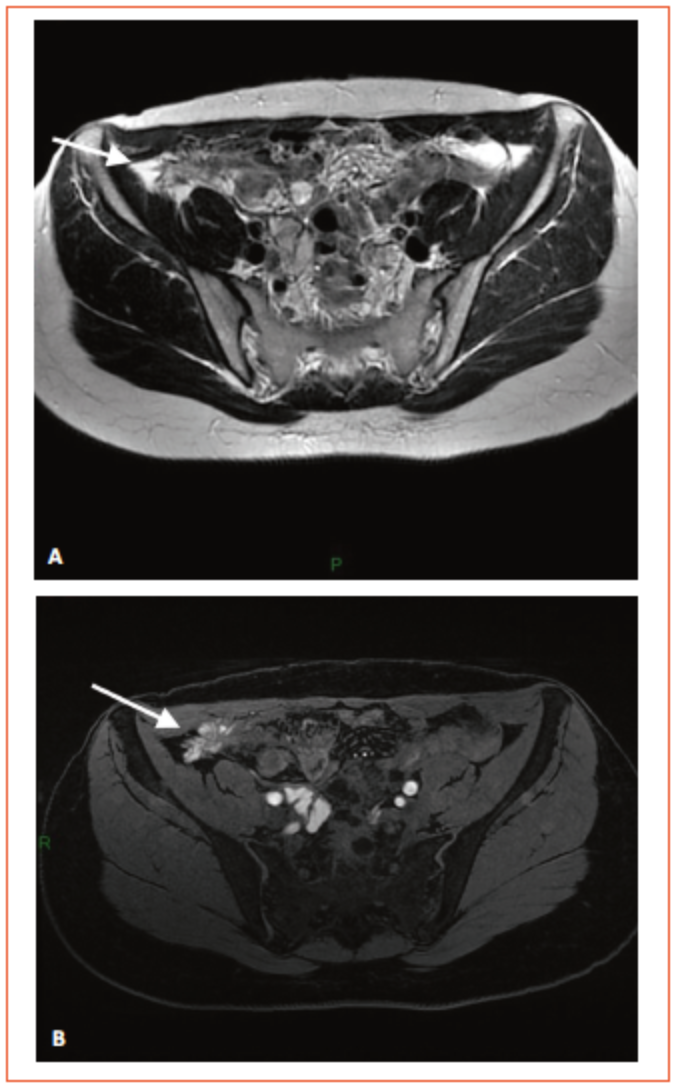
Figure 8: Lower cecal bottom in a patient with multifocal digestive endometriosis. A. Spicular damage in T2 axial sections (white arrow).B. Hypersignal hemorrhagic implants T1 with fat saturation (white arrow).
Conclusion
The MRI is now a key tool in the diagnosis and assessment of the extent of endometriosis. It allows the clinician to accurately assess the locations and extent of the disease in order to accurately determine the optimal treatment, surgical or medical, to provide the best possible relief to patients in terms of pain, quality of life or fertility.
References
Click on the references and access the Abstracts on

1. Bazot M, Gasner A, Lafont C, Ballester M, Daraï E. Deep pelvic endometriosis: limited additional diagnostic value of postcontrast in comparison with conventional MR images. Eur J Radiol 2011 ; 80 : e331-9. Search the abstract2. Bazot M et al. Comparison of 3D and 2D FSE T2-weighted MRI in the diagnosis of deep pelvic endometriosis: preliminary results. Clin Radiol 2013 ; 68 : 47-54. Search the abstract3. Bazot M et al. Value of thin-section oblique axial T2-weighted magnetic resonance images to assess uterosacral ligament endometriosis. Hum Reprod 2011 ; 26 : 346-53. Search the abstract4. Bazot M et al. Diagnostic accuracy of physical examination, transvaginal sonography, rectal endoscopic sonography, and magnetic resonance imaging to diagnose deep infiltrating endometriosis. Fertil Steril 2009 ; 92 : 1825-33. Search the abstract5. Bazot M et al. The value of MRI in assessing parametrial involvement in endometriosis. Hum Reprod Oxf Engl 2012 ; 27 : 2352-8. Search the abstract
Articles on the same theme
- 1 of 2
- >